4 Ways Simulation Can Assess Foundational Competencies
Learn how simulation can be a powerful tool for ensuring readiness for residency in medical education.

Learn how simulation can be a powerful tool for ensuring readiness for residency in medical education.

If you’re in undergraduate medical education, you may know that the Association of American Medical Colleges (AAMC), the American Association of Colleges of Osteopathic Medicine (AACOM), and the Accreditation Council for Graduate Medical Education (ACGME) are working together to create a set of foundational competencies for undergraduate medical education programs in the U.S. Due to be released in early 2024, these medical school competencies will aim to improve the transition to residency.2 To help inform the development of the foundational competencies, members of the medical education community have contributed their input on the skills they believe are essential.3
In this article, we discuss 4 of these skills and how simulation can help you teach and assess them to ensure that you’re preparing your learners to provide safe, effective patient care upon their transition to residency.

According to the Accreditation Council for Graduate Medical Education (ACGME), the goal of assessing learners’ application of medical knowledge is to assess their ability to apply that knowledge to clinical problem-solving and clinical reasoning – the process where clinicians observe, collect, and interpret data to diagnose and manage patients.4 This ability to transfer knowledge to practice is critical for safe and effective patient care – but has shown to be a struggle for many learners.5
In a survey of 123 Clerkship Directors in Internal Medicine, the majority of respondents felt that most students enter their clerkships with only poor to fair knowledge of key clinical reasoning concepts.6 And, most respondents agreed that a structured curriculum in clinical reasoning should be taught throughout the 4 years of medical school.7
Simulation has been touted as an essential tool in assessing clinical reasoning thanks to its ability to measure the "whole task" – or the full range of clinical reasoning components, from information gathering to differential diagnosis to management and treatment.8 Whole-task assessments are essential for providing learners with formative feedback to foster clinical reasoning.9
Simulation assessment tip:
Ensuring your learners can successfully apply their knowledge to patient care will require offering many opportunities to practice and master this skill across the curriculum. Simulation lends the ability to do this in a safe, consistent environment. To measure and track learner progress longitudinally, consider enlisting the help of a simulation management system. SimCapture can collect and organize your performance data to yield trends and insights that can help you adjust your teaching as needed.
This skill aligns with Core Entrustable Professional Activity (EPA) 1: Gather a History and Perform a Physical Examination.10 Developed by the Association of American Medical Colleges (AAMC) in 2014, the EPAs are a set of behaviors that graduating medical students should be able to perform with indirect supervision upon entry to residency.11
In a 2017 survey of Internal Medicine program directors, 97% of respondents said this is one of their top 3 essential EPAs for new residents to possess on their first day.12
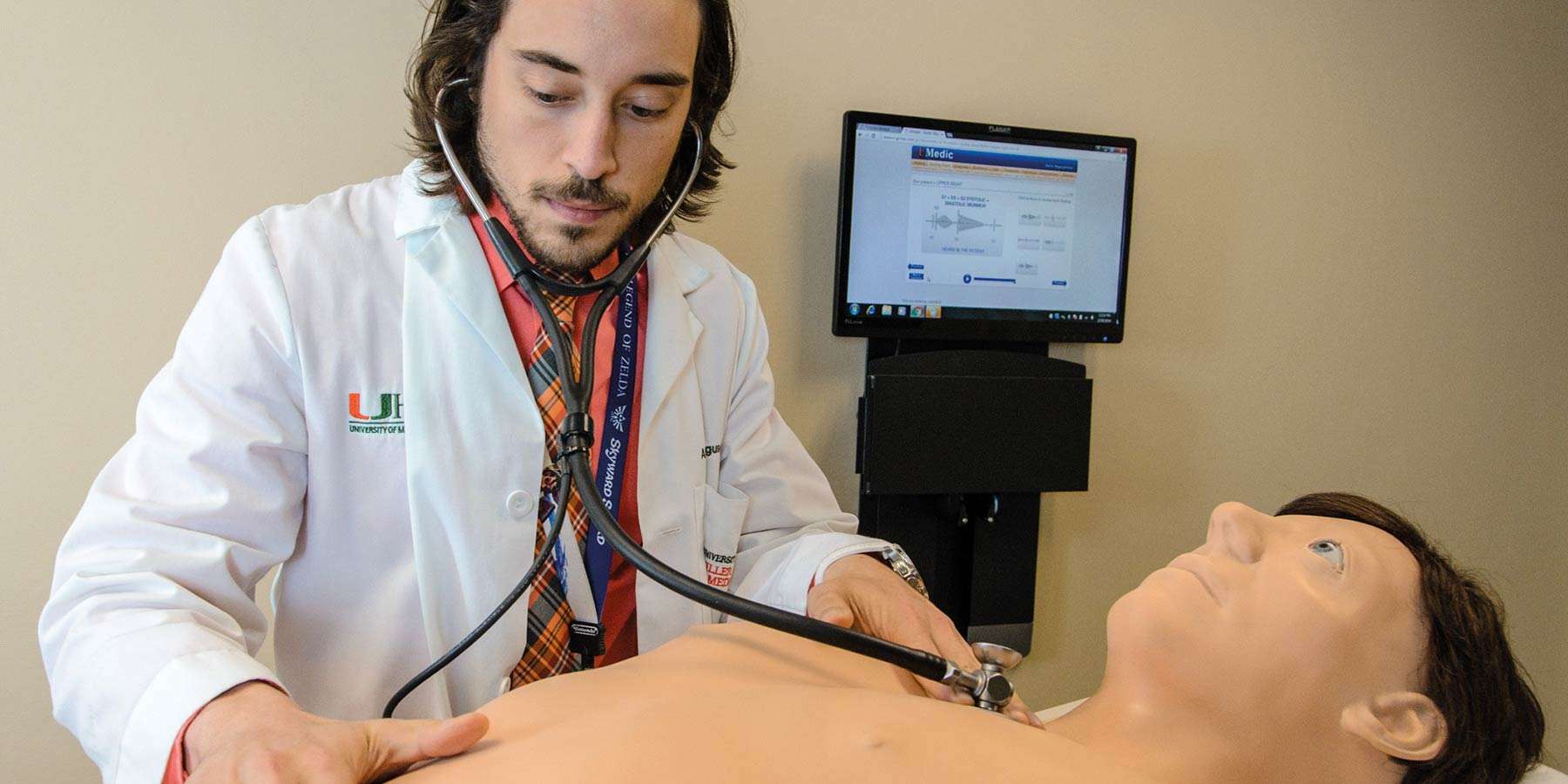
According to the AGCME, simulation is becoming increasingly important as part of mastery-based learning for patient care skills, including taking a patient history and conducting physical assessment.13 Mastery learning, when paired with deliberate practice, has been shown to yield significant educational outcomes.14
- Dr. Sandrin van Schaik, MD, PhD
Kanbar Center for Simulation and Clinical Skills, University of California San Francisco Medical School15
One specific type of physical assessment that especially illustrates the importance of deliberate practice is cardiopulmonary assessment. This complex exam demands the integration of inspection, palpation, and auscultation in the context of initial symptoms and the patient’s history.16
One study looked at 4th year medical students’ bedside cardiology skills.17 Students engaged in deliberate practice of cardiac findings with computer-based teaching modules linked to cardiopulmonary simulator Harvey. They nearly doubled their baseline scores post-test – in half the time as the comparison group, who practiced using customary ward work such as teaching rounds. This study illustrates that simulation technology that engages learners in deliberate practice of clinical skills results in significant improvements in a relatively short time, with little faculty involvement.18
Simulation assessment tip:
Deliberate practice is vital to helping learners master their skills in taking a patient history and conducting a physical assessment – but not every student prefers to practice and learn in the same environment. Consider utilizing a simulator that allows learners to deliberately practice skills like cardiopulmonary assessment in an instructor-led, peer-to-peer, or self-directed environment – while also providing feedback and yielding performance data on their skill development.

This skill aligns with Core Entrustable Professional Activity (EPA) 9: Collaborate as a Member of an Interprofessional team.19
Teamwork and collaboration are considered “soft” skills – even though they are anything but soft in reality.20 Effective teamwork enhances safety, efficiency, and quality of patient care.21
The Joint Commission’s 2022 Annual Review of Sentinel Event Data indicated that communication breakdowns (including not establishing a shared understanding or mental model across care team members or no or inadequate team communication of crucial information) continue to be the leading factor contributing to sentinel events.22
A well-designed simulation scenario allows students to learn how to work well together without posing any risk to actual patients. At the University of Missouri, teams of students from the medical, health management, pharmacy, respiratory therapy, and nursing schools participate in a simulation of an emergency department during a flu epidemic. Students are observed not only on what they’re doing but on how well they work together.23
- Dr. Linda Headrick, M.D., Senior Associate Dean for Education
University of Missouri-Columbia School of Medicine24
Simulation assessment tip:
According to the ACGME, it is especially critical to use a multisource feedback (MSF) approach when assessing interprofessional teamwork.25 This approach provides multiple perspectives, which may offer a more holistic assessment of skills.26 You may want to consider making this process easier with a video debriefing tool like SimCapture, which provides video recordings along with annotations, allowing multiple faculty to view footage and assess learners.

This skill aligns with Core Entrustable Professional Activity (EPA) 10: Recognize a Patient Requiring Urgent or Emergent Care and Initiate Evaluation and Management.27
New residents are often the first to respond in an acute care setting or to be notified about an abnormal lab or deteriorating patient.28 Yet research has shown that fourth-year medical students are less prepared to handle unstable patients than patients with non-acute conditions.29 This could be due in part to the reality that most students don’t encounter enough emergent conditions in patient encounters during an emergency medicine rotation.30
And, certain emergent conditions (especially cardiac arrest) are much less likely to be encountered.31
Simulation can expose students to realistic emergent conditions that they might not otherwise encounter without any impact on patients in an actual emergency. And, it adds standardization to training by ensuring that every learner gets the same experience.
Many organizations are turning to Virtual Reality (VR) medical simulation for its ability to immerse learners in real-world environments that allow them to practice recognizing emergencies. And, it provides training on multiple skills, including teamwork – an area especially critical in a time-critical emergency. In this virtual world, a student can encounter a patient with chest heaviness, recognize that the patient requires urgent care, and initiate evaluation and management while engaging actual team members, before moving on to managing a full cardiac arrest – all in a single scenario.
For Linda Boyd, D.O., Vice President for Academic Affairs and Dean at West Virginia School of Osteopathic Medicine, one of the most important strengths of VR simulation is its ability to give learners practice in communicating effectively – particularly with patients’ families. “Since medicine is much more than just giving the right drugs and doing the right tests, being able to interact in a realistic and complex scenario is valuable for medical students learning their craft,” she says.32
Simulation assessment tip:
VR simulations can help you increase opportunities for deliberate practice of emergency recognition and other key skills like teamwork. To help with assessment, you may want to consider a VR platform that offers robust performance data – including reports of critical actions performed and timestamps of when they happened. These tools can make it easier to review performance with your learners, provide meaningful feedback, and track their progress over time.