How to Use Simulation to Promote Healthcare Equity
Learn from the leaders.

Learn from the leaders.

Are your simulations effectively preparing your learners to provide equitable care for diverse populations?
We sat down with three experts on the topic of using simulation to promote healthcare equity. During the 90-minute round table, these luminaries shared a multitude of insights and advice that you can incorporate into your simulation program.
Read below for some highlights from the discussion. Then, plan to set some time aside to watch the full webinar on-demand: A Call-for-Action: Simulation as a Means to Achieve Healthcare Equity.
Dr. Crystal Murillo, PhD, RN, CHSE-A, ANEF, FAAN, Assistant Dean of Simulation and Assistant Professor at the University of South Carolina, explained that the role of social justice and healthcare equity in simulation curricula ties back to the common goal that all healthcare providers should share: quality healthcare for every individual. Simulations should be designed to reflect that goal from conceptualization to evaluation, she advised. "We should be focused on equity because it meets people where they are."
- Dr. Crystal Murillo, PhD, RN, CHSE-A, ANEF, FAAN

"Simulation should mimic what’s happening outside, or what should be happening outside, in our community," added Dr. Desiree Díaz, PhD, FNP-BC, CNE, CHSE-A, ANEF, FSSH, FAAN, Associate Professor at the University of Central Florida. "It’s a prime place for us to model the behavior we want to see in future healthcare providers."

Throughout the discussion, the experts kept going back to the importance of intentionality. This means being clear and purposeful about what we want our learners to gain through the simulation experience.
Dr. Kellie Dionne Bryant, DNP, WHNP, CHSE, FAAN, Assistant Dean of Clinical Affairs and Simulation and Associate Professor at Columbia University School of Nursing, explained that the goal shouldn’t be to just check a box that we’ve included a certain race, for example, in a scenario. Instead, it’s important to be purposeful when incorporating those elements.
- Dr. Kellie Dionne Bryant, DNP, WHNP, CHSE, FAAN

Addressing sensitive topics that may be uncomfortable for both learners and facilitators to talk about will require repetition. "The only way to increase 'comfortability' is to keep having these conversations over and over again," advised Kellie.
"People don’t change perceptions with a single experience," Crystal said. "It takes repeated exposure because there's something happening in the brain."
She explained that our brains cause us to gravitate to where we’re comfortable. In an uncomfortable situation, she explained, there's a “reptilian” part of the brain that doesn’t want to respond because it isn’t comfortable or used to being exposed to that kind of situation. Intentionally exposing us to these types of conversations allows our brains to enter into deeper levels of cognition and reasoning.
"We really have to lean into and support people when they’re feeling this brain response. Because that’s how we move from not being aware or being biased, to not being biased," she said.
"It should be scaffolded," Desiree added. "You can’t just say this is important content and plop it in once."
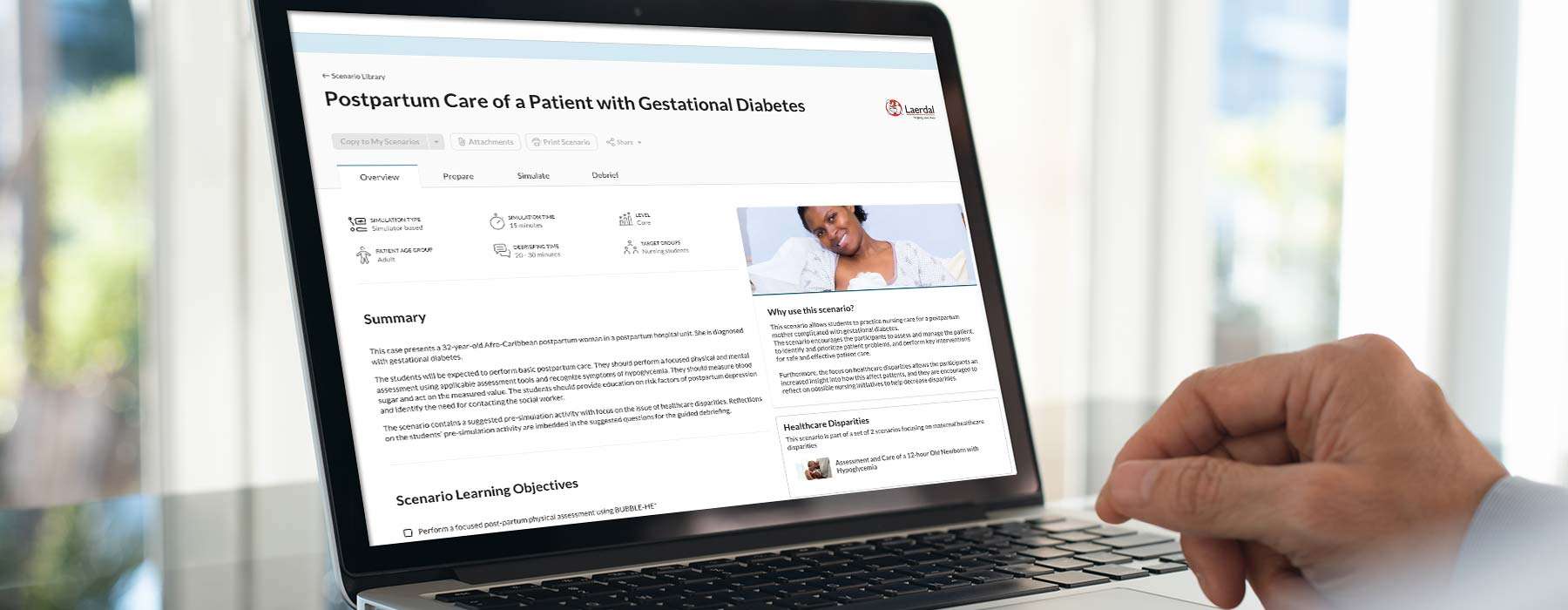
Some of the resources and tools that the experts talked about included:
During the webinar, the audience weighed in on where they find diverse scenarios:
create their own
use real events or experiences to guide their scenarios
use textbooks and literature to support their scenario design
download them from various resources

Crystal asserted that the simulation science tells us how to do simulation well:
Crystal also recommended focusing on quality health indicators. She shared that she’s obtained grants by taking data on quality health indicators specific to her region and articulating how simulation will serve as an intervention to inform learners how to address them.
Desiree shared that she’s also been able to secure grants by taking the highest Diagnosis Related Groups (DRGs) or hospital admission rates and pointing out that, "We can’t guarantee that every student is going to get a COPD [or] a stroke patient – but we can in sim. So we're going to use those to make our students solid for the communities they serve."
Kellie explained that she works with course instructors in using student performance data to identify areas where she can help fill in gaps. If there are areas students are struggling with or there isn't enough time to cover something in depth, she said, "Let me build a simulation to help enforce that learning."

The experts agreed that finding and joining forces with others in your organization who are willing and interested is a low-hanging fruit strategy – and a good place to get started.
Kellie shared that taking this approach allowed her to eventually piece together a committee consisting of other "champions" in her department and the hospital. "Find those other people that are interested in the same topic, band together…and work on a plan," she encouraged.
- Dr. Desiree A. Díaz, PhD, FNP-BC, CNE, CHSE-A, ANEF, FSSH, FAAN
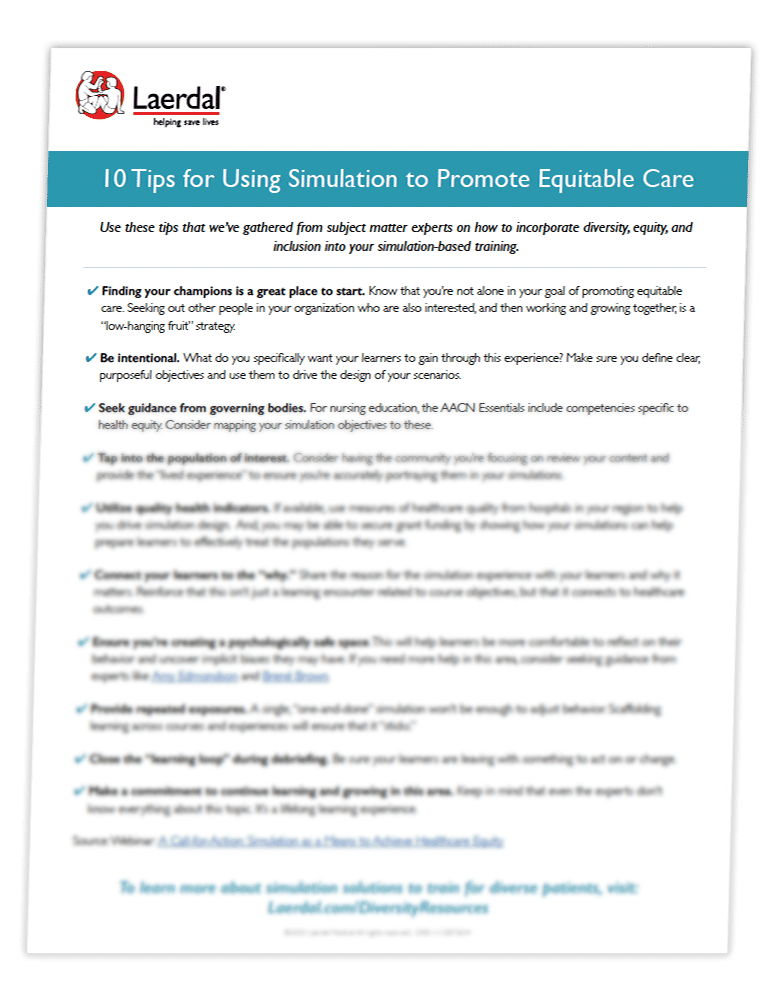
Want a list of tips for making your simulations more diverse?
Use this checklist of expert-provided advice to help you ensure you’re effectively preparing your learners to provide equitable care.

Dr. Kellie Dionne Bryant DNP, WHNP, CHSE, FAAN
Dr. Desiree A. Díaz PhD, FNP-BC, CNE, CHSE-A, ANEF, FSSH, FAAN

Dr. Crystal Murillo PhD, RN, CHSE-A, ANEF, FAAN
Dr. Kellie Bryant is currently the Assistant Dean of Clinical Affairs and Simulation and Associate Professor at Columbia School of Nursing’s accredited Helene Fuld Health Trust Simulation Center. She also is a consultant for Dr. Uché Blackstock’s Advancing Health Equity company. Dr. Bryant has over 20 years of teaching experience and 15 years of experience in simulation. Throughout her career, she has become an expert in the field of simulation through her experience with designing simulation centers and implementing simulation programs for two of the top-rated nursing schools in the country. In her current role, she oversees the day-to-day operations and implementation of simulation-based education for all the prelicensure and advanced practice nursing students. She is also the medical director of Columbia’s Opioid Overdose Prevention Program, which has provided training to over 2,000 individuals. Additional responsibilities include implementing institutional and community-based initiatives that promote diversity, equity, and inclusion.
Dr. Bryant’s research focus includes simulation use to improve patient safety, opioid overdose prevention, and developing nursing pathway programs for historically marginalized students. Her work has been disseminated globally through 1) 23 published articles, 2) research as Primary/Co-Investigator for over $5,659,000 in research projects and 3) conducting over 100 presentations.
Dr. Bryant serves on many national and international committees. At Columbia University, she was appointed co-chair of the campus-wide antiracism task force for community service. She is currently the chair of the Society for Simulation in Healthcare’s (SSH) media and communication committee, appointed member of SSH’s DEI workgroup, member of the International Nursing Association of Clinical Simulation Learning IncluDE diversity committee, and serves on the editorial board for the Clinical Simulation in Nursing journal. She is serving her third year on the CDC-funded Nurse-Led Vaccine Confidence Advisory Committee. Lastly, Dr. Bryant is currently on the executive board of the Greater NYC Black Nurses Association, including serving as the liaison for the NYC Black and Latinx Providers task force.
She received her Associate's degree in nursing from Hudson Valley Community College. She continued her education at Stony Brook University where she received her Bachelor’s in Nursing and a Master’s Degree as a Women’s Health Nurse Practitioner. Lastly, she received her Doctorate in Nursing Education from Case Western Reserve University.
Dr. Desiree A. Díaz is the Undergraduate Simulation Coordinator and an Associate Professor at the University of Central Florida. She completed a Post Doc from Johns Hopkins with Dr. Pamela Jeffries, which focused on simulation pedagogy. Dr. Diaz creates tests and disseminates research on cutting-edge technologies such as holograms within the simulation community. Her strategies within simulation research pedagogy over the last decade have promoted health equity and brought awareness to healthcare disparities. She was a National Coalition Ethnic Minority Nurse Scholar and Health Leadership Fellow. She serves as President-elect of the International Nursing Association for Clinical Simulation.
Her current grant funding focuses on educating and exploring ways to eliminate healthcare disparities while educating the workforce. As co-PI to a 2.7 million dollar HRSA grant “ENFERMERIA” which looks to empower and enhance linguistic services and culturally congruent care within the Hispanic community while encouraging advancement to graduate degrees of diverse post-baccalaureate student populations and as PI on approximately $500k grant that utilizes simulation to examine healthcare disparities and the role of public health nursing, Dr.Diaz engages multiple means to reduce healthcare inequity and encourage healthcare equity advocates.
Dr. Crystal Murillo (previous surname Graham) is an academic nurse scientist and simulationist with a tripartite portfolio focused on using simulation to prepare nursing students to view themselves as social justice advocates for health equity. Her research, teaching, and service activities revolve around the social determinants of health and learning and improving outcomes for underrepresented and minoritized nursing students and faculty. She has served as a principal investigator for $1.1 million in grant funding to lead nursing faculty in restructuring simulation curricula to focus on the preparation of a critically conscious future nursing workforce. Based on this work, she was invited to speak at the National Academy of Medicine (NAM) - the inaugural nurse from the state of South Carolina invited to speak at the Academy. Dr Murillo is a founding member and the current President of the South Carolina Nursing Education Simulation Alliance (SCNESA). She is also adjunct faculty for the Harvard Center for Medical Simulation. In 2022, Dr Murillo was elected to serve on the Board of Directors for the International Nursing Association for Clinical Simulation and Learning (INACSL). In the same year, she was inducted as a fellow in both the NLN Academy of Nursing Education (ANEF) and the American Academy of Nursing (FAAN).
Sign up for Laerdal Medical email updates. You can identify your interests and receive new educational content, updates, event information and more.