Ultrasound isn’t just used in maternal care practices. Having come a long way since its roots in military and industrial settings, today ultrasound is well-established as a crucial technology across a range of diagnostic and therapeutic applications. The uses vary from determining the size and sex of a fetus to boosting the accuracy of a needle biopsy to treating a soft-tissue injury. Further, bedside point-of-care ultrasound (POCUS) has evolved into a valuable addition to an acute care clinician’s toolbox in settings such as emergency and intensive care medicine. It’s fast, improves diagnostic accuracy and informs treatment plans by condensing the list of viable diagnostic etiologies.1
Herein, we discuss the applications of point-of-care ultrasound as well as why you might want to consider integrating it into your existing simulations.
POCUS: The Need to Know
Acting as one large piece of the diagnostic puzzle, POCUS findings typically indicate the next step in the care pathway.
POCUS can help reinforce core anatomy and physiology concepts, illustrate pathology and disease processes, and facilitate mastery of the physical examination. For these reasons, organizations ranging from the American Academy of Emergency Medicine to the American Institute for Ultrasound in Medicine, have advocated for POCUS as an important element of undergraduate medical education. 2 3
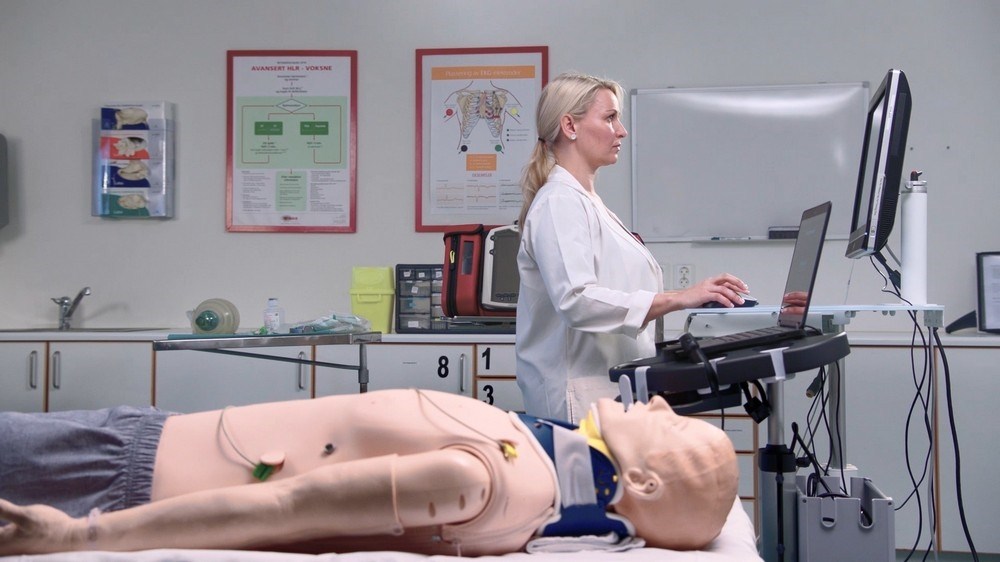
However, there are two caveats. First, POCUS is operator dependent. Confidence and competence in image acquisition and interpretation are essential, as is the ability to incorporate one’s findings into clinical decision-making.4 Developing the necessary operator competence in ultrasound often proves problematic, as it currently consists of a “see one, do one” approach that requires patients, standardized patients, commercial training models or cadavers — all at substantial cost.
Second, today’s ultrasound training typically lacks an emphasis on critical thinking and decision-making components — vital in emergency and intensive care settings.