3 Powerful Benefits of Interprofessional Cardiac Arrest Simulation Training


– Jennifer McCarthy, MAS, NRP, CHSE-A
Director of Clinical Simulation at Seton Hall University
President/Founder of 579 Solutions
Former Paramedic Science Program Director

During high-acuity emergencies like out-of-hospital cardiac arrest (OHCA), seamless coordination among clinicians is critical to maintaining strong links in the chain of survival. Yet, teams often train in silos.
Interprofessional healthcare simulation training is a form of interprofessional education in healthcare (IPE). Interprofessional education in healthcare (IPE) is commonly described as “health professionals from two or more backgrounds learning with, from, and about each other.”1 Interprofessional cardiac arrest simulation training provides a risk-free opportunity for teams to come together to train for OHCA emergencies.
In this article, we discuss three powerful benefits you can reap from using interprofessional cardiac arrest simulation training to ensure your teams are prepared to effectively respond to OHCA emergencies.

An efficient hand-off from EMS to the Emergency Department (ED) is especially critical during an emergency like OHCA, where every second is critical.4 Patients experiencing OHCA have a higher chance of survival if there is a strong link between prehospital care and in-hospital care.5
Yet hand-offs are often disorganized and chaotic, riddled with interruptions like noise and repeated questions.6 In many cases, there is no standardization for hand-off reports from EMS to the ED for OHCA patients, and communication is variable.7 One study found that key information doesn’t get communicated in up to 86% of OHCA hand-offs.8
A 2023 study involving over 13,000 patients found that initiatives to improve teamwork in multidisciplinary healthcare teams can reduce patient mortality by 28%.9 Simulation-based team training has been found to help create stronger teams by improving communication, teamwork, and leadership.10
– Sarah L. Beebe, PhD, APRN, CNM, WHNPr, CHSE
Graduate Medical Education Simulation Lab Program Manager
Bayhealth Medical Center


A 2023 report looked at the factors impacting treatment of OHCA. They gathered the perspectives of emergency responders, including 911 telecommunicators, law enforcement, firefighters, and EMS personnel.11
The respondents agreed that relationships between different stakeholders within the response system have a major impact on teamwork in an OHCA.12 They suggested that improving understanding of different roles could help improve these relationships.13
In the report, one EMS provider expressed that, “Many nurses and doctors say, ‘How come you guys didn’t do this?’ [I say] ‘Do you realize the size of the room we work in? In an ambulance and/or the environment, leaning up against the wall?’ I think there’s a disconnect there … we are not a lot of hands and in some very precarious environments. I wish there was a way to get that education to some of the people that we work closely with.”14
When teams come together for cardiac arrest simulation scenarios instead of training in silos, they can better understand each other’s realities. Simulation provides the perfect opportunity to do this in a safe, risk-free environment.
“By being side-by-side in simulation … [we’re] slowing down to actually honor everybody’s role in that rushed environment,” explains Jennifer McCarthy, MAS, NRP, CHSE-A, Director of Clinical Simulation at Seton Hall University, President/Founder of 579 Solutions, and former Paramedic Science Program Director.
Winona Health, a healthcare system in Winona, Minnesota, regularly brings in the local EMS, paramedics, and fire departments for interprofessional simulation training.
"It’s a great way to start to integrate different kinds of caregivers and begin to understand the perspective of someone else," explains Karla Eppler, ME-PD, NRP, former Director of Learning and Development at Winona Health.
– Karla Eppler, ME-PD, NRP
Former Director of Learning and Development at Winona Health


Simulation has been shown to help healthcare systems effectively test and refine new resuscitation protocols before using them on actual patients.16
In 2024, the city of Boston, Massachusetts created a city-wide initiative for Extracorporeal Cardiopulmonary Resuscitation (ECPR). ECPR involves the initiation of venoarterial extracorporeal membrane oxygenation (ECMO) in patients experiencing cardiac arrest.17
They brought together EMS personnel and two hospital-based teams (emergency medicine and ECMO) for a high-fidelity in situ simulation (or simulation occurring in the actual work environment). They focused on uncovering systems issues and opportunities where they could improve the new protocol.
To maximize the cardiac arrest simulation scenario’s fidelity for the participants, they chose to use the MegaCode Kelly™ manikin. The manikin allowed for endotracheal intubation, defibrillation, intravenous and intraosseous medication administration, and the application of a mechanical chest compression device.
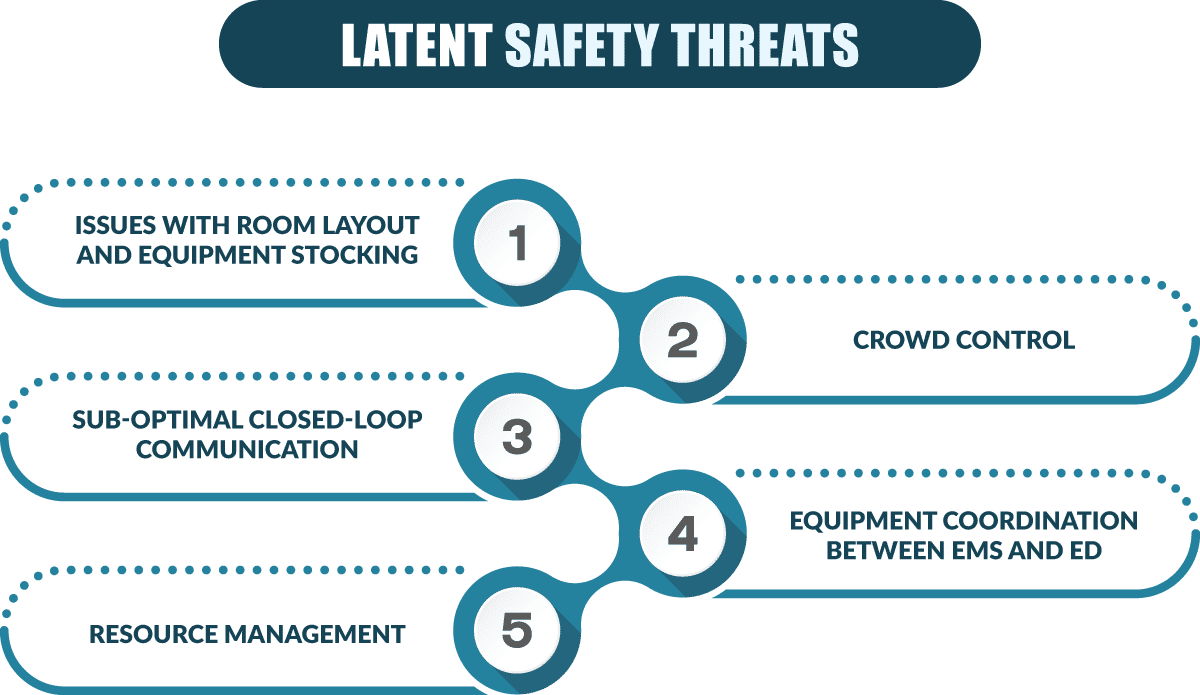
By bringing these teams together for an interdisciplinary in situ simulation with a structured debriefing, they were able to uncover numerous latent safety threats (or accidents waiting to happen) – in areas including:
A single well-designed interprofessional simulation scenario can test and improve the response to OHCA across the entire chain of survival. Consider this scenario example:
The simulation follows a 58-year-old male's OHCA in a shopping center parking lot. The scenario begins with a 911 dispatcher providing telephone-assisted CPR instructions to a bystander, followed by a police officer’s arrival for initial scene management and CPR continuation. Fire department personnel then deploy advanced equipment, including AED and oxygen support, before EMS arrives to provide advanced cardiac life support (ACLS) and coordinate transport. The simulation concludes with a structured hand-off to the emergency department team.
Throughout each transition, participants practice critical hand-off communications while experiencing the unique challenges and perspectives of each discipline – from dispatchers managing multiple emergency calls to police officers balancing medical care with scene safety, and from firefighters transitioning between rescue and medical roles to paramedics making complex transport decisions.
Interprofessional simulation training isn’t just a “nice to have.” It’s a must for building the type of collaborative culture that saves lives. Simulation offers a rare chance to break down silos, sharpen team performance, and ultimately, make a positive impact on outcomes from OHCA.
Whether you’re planning your first interprofessional simulation or expanding your program, keep one thing in focus: the best care happens when disciplines train – and grow – together.
1. Naike Bochatay, Ju, M., O’Brien, B. C., & Schaik, van. (2024). A Scoping Review of Interprofessional Simulation-Based Team Training Programs. Simulation in Healthcare. https://doi.org/10.1097/sih.0000000000000792
2. Howell, D. M., Margius, D., Li, T., Cohen, A. L., McCann-Pineo, M., Haddad, G., Becker, L., Young, E. A., Rolston, D. M., & Jafari, D. (2023). Emergency Medical Services handoff of patients in cardiac arrest in the Emergency Department: A retrospective video review study of duration and details of handoff. Resuscitation, 189, 109834. https://doi.org/10.1016/j.resuscitation.2023.109834
3. Ibid.
4. Ibid.
5. Handover of the out-of-hospital cardiac arrest patient from prehospital to in-hospital care: A guideline from the Dutch Resuscitation Council. (2022). Dutch Resuscitation Council. Retrieved from https://www.reanimatieraad.nl/app/uploads/2022/11/Guideline-Handover-of-the-out-of-hospital-cardiac-arrest-patient-from-prehospital-to-in-hospital-care.pdf
6. Howell, D. M., Margius, D., Li, T., Cohen, A. L., McCann-Pineo, M., Haddad, G., Becker, L., Young, E. A., Rolston, D. M., & Jafari, D. (2023). See reference #2.
7. Ibid.
8. Ibid.
9. Weller, J. M., Mahajan, R., Fahey-Williams, K., & Webster, C. S. (2024). Teamwork matters: team situation awareness to build high-performing healthcare teams, a narrative review. British Journal of Anaesthesia, 132(4), 771–778. https://doi.org/10.1016/j.bja.2023.12.035
10. Murphy, M., Curtis, K., & McCloughen, A. (2016). What Is the Impact of Multidisciplinary Team Simulation Training on Team Performance and Efficiency of Patient care? an Integrative Review. Australasian Emergency Nursing Journal, 19(1), 44–53. https://doi.org/10.1016/j.aenj.2015.10.001
11. Missel, A. L., Dowker, S. R., Dzierwa, D., Krein, S. L., Coulter-Thompson, E. I., Williams, M., Trumpower, B., Swor, R. A., Hunt, N., & Friedman, C. P. (2023). Factors Impacting Treatment of Out‐of‐Hospital Cardiac Arrest: A Qualitative Study of Emergency Responders. Factors Impacting Treatment of Out-of-Hospital Cardiac Arrest: A Qualitative Study of Emergency Responders, 12(10). https://doi.org/10.1161/jaha.122.027756
12. Ibid.
13. Ibid.
14. Ibid.
15. Ibid.
16. Jansson, P. S., Underiner, R., Baymon, D. E., Eyre, A. J., & Seethala, R. R. (2025). Multiorganizational and multidisciplinary high-fidelity simulation of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Journal of EMS Medicine. https://doi.org/10.35616/jemsm.2024.00115
17. Ibid.