3 Tips for Using Simulation to Build and Assess Competence in EMS Providers


Whether you’re preparing students for their first patient encounter or helping seasoned providers sharpen their skills, one thing remains constant: competence isn’t built by lectures alone. It’s earned through hands-on, realistic, and data-informed practice — and that’s where simulation shines.
Simulation lends a unique opportunity to replicate the complexity, unpredictability, and emotional intensity of real-world prehospital care. It not only builds psychomotor skills, but also develops the judgment, adaptability, and confidence that providers need to perform under pressure.
Even more importantly, it creates a structured environment for assessment: educators can evaluate performance objectively, give targeted feedback, and verify competency over time.
In this article, we explore three high-impact ways to use simulation to build and assess essential competencies — from soft skills to CPR to community births — in your pre-hospital training program.

Soft skills — such as communication, teamwork, resilience, adaptability, and clinical reasoning — are among the most difficult competencies to teach, but they are often what separate a good EMS provider from a great one.
These skills come into play when providers face unexpected challenges: a combative patient, a malfunctioning piece of equipment, or limited resources on scene. They also shape how providers communicate with patients and families, coordinate care with partners, and make decisions under stress.
How to teach and assess soft skills with simulation:
Assessment tip: A high-fidelity manikin like SimMan® ALS allows you to create complex, dynamic scenarios that challenge learners’ decision-making and adaptability — from sudden patient deterioration to unanticipated equipment failure.
Recording your scenarios with a simulation video recording system allows learners to watch their own performance, reflect on communication and teamwork behaviors, and understand how their decisions unfolded in real time. Having the performance data also helps you objectively assess soft skills and track growth over time.
- Ed Biebel
Clinical Simulation Manager, Rowan College at Burlington County
Related Reading: Preparing Paramedic Students with Video-Assisted Debriefing at Rowan College
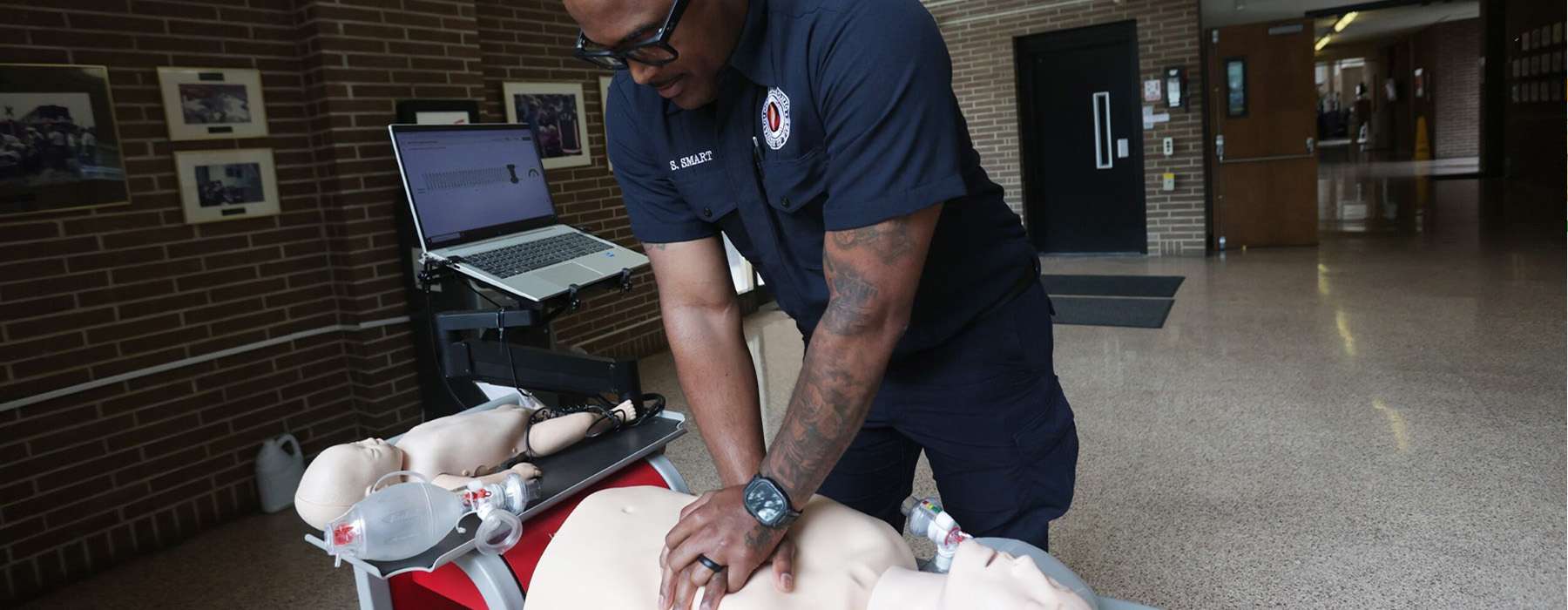
CPR is one of the most fundamental — and most perishable — EMS skills. While many providers initially master chest compressions and ventilations during certification, competence often declines without regular, deliberate practice.
Traditional skills refreshers, typically conducted once or twice a year, are not enough to maintain high-quality performance. Research shows that low-dose, high-frequency training — shorter, more frequent practice sessions — is more effective for skill retention and performance.
How to teach and assess CPR with simulation:
Assessment tip: Optimal CPR simulation tools provide real-time feedback and performance data that can be stored, analyzed, and used to verify competency for both initial certification and ongoing education.
Programs like Resuscitation Quality Improvement® (RQI®) and HeartCode® Complete deliver scenario-based CPR training combined with objective performance feedback. These platforms continuously measure and report learner performance — helping you verify that providers meet evidence-based benchmarks for CPR quality.
And, the platforms manage providers’ American Heart Association (AHA) certifications and renewals.
- Firefighter Robert Kelley,
EMS Training Specialist and AHA Training Center Coordinator, Columbus Division of Fire
Related reading: Advancing CPR Training with RQI® at Columbus Division of Fire

Few situations test a pre-hospital provider’s composure and clinical skills like an unexpected out-of-hospital birth. These calls require rapid assessment, clear communication, and confident execution of skills that many providers don’t get to practice often.
Simulation offers a safe way to prepare learners for the full spectrum of obstetric emergencies — from uncomplicated deliveries to shoulder dystocia and postpartum hemorrhage.
How to teach and assess obstetric competence with simulation:
Assessment tip: When training for obstetric emergencies, document not only procedural competence but also decision-making and communication under stress. Use structured debriefing to help reinforce lessons and improve performance.
A maternal and birthing simulator gives learners hands-on experience with realistic out-of-hospital birth scenarios — including complications that require rapid clinical reasoning and teamwork. Combine it with a simulation management system like SimCapture™ for EMS to record scenarios, analyze team dynamics, and provide detailed feedback that accelerates competence and improves future performance.
For programs looking for a more cost-effective training option, MamaBirthie offers hands-on practice in essential birthing maneuvers while maintaining respectful maternity care.