The Role of Low-Fidelity Simulation in Labor and Delivery
Improving Maternal and Newborn Care
Simulating birth scenarios can help healthcare professionals recognize and potentially mitigate adverse events for new mothers and newborns.1 However, the degree of realism or "fidelity" chosen for those scenarios does not always have to be extreme. Often when educators begin to plan scenarios around labor and delivery, their strategy jumps quickly to high-fidelity, full-bodied birthing simulators. But, depending on the learning goals, the effort required to plan and set up a high-fidelity simulation can be unnecessary and labor-intensive.
Low-fidelity simulation can provide learners with a wealth of training experience – at minimal expense. Below, we sum up three ways that you can use low-fidelity simulation training to reduce preventable harm to maternal and newborn patients.
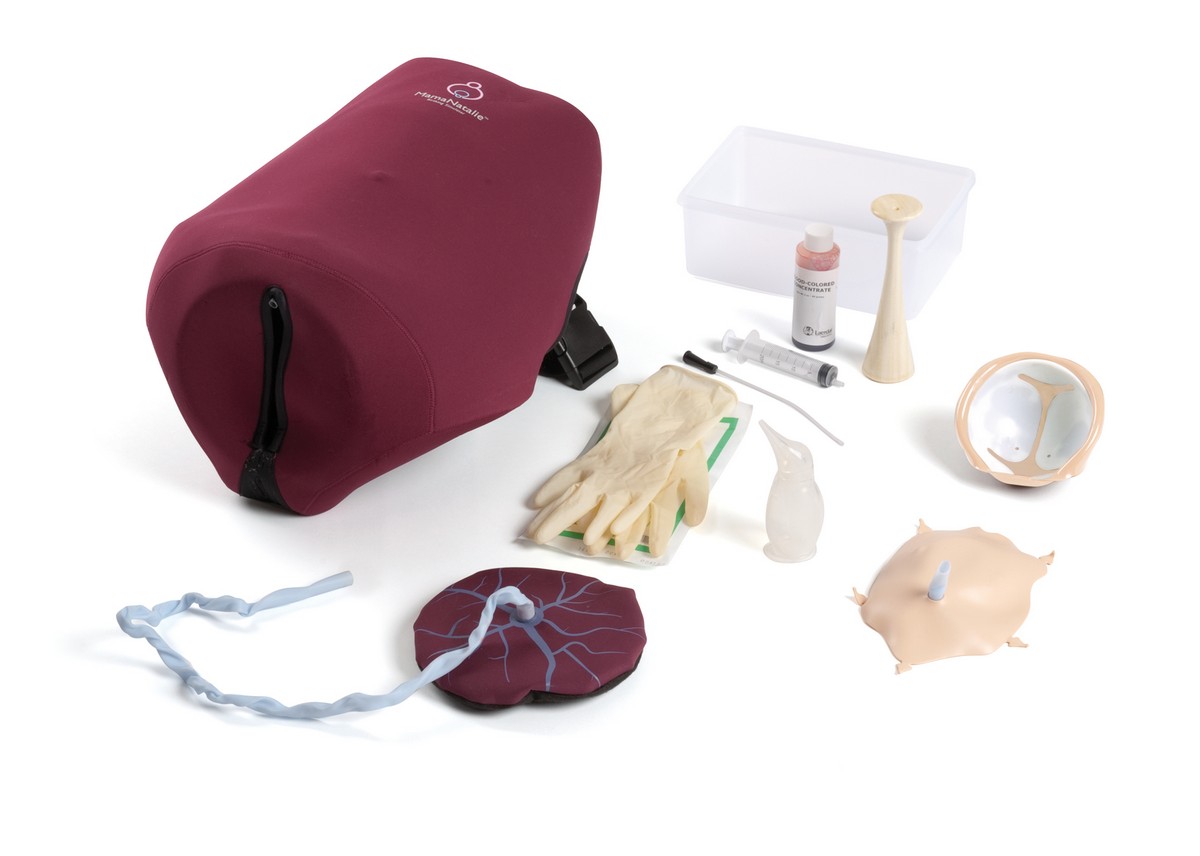
Task Trainers – How Your Learners Can Improve Skills Performance
Situations that require repeated practice are best suited for use of a task trainer. For example, a great opportunity to use a task trainer is in the training of birthing assessments and different delivery protocols. Learners can practice hands-on, psychomotor skills independently and at their own pace without the complexity of a high-fidelity simulation.
In a study evaluating the training of shoulder dystocia using a birthing simulator, learners saw a 44% improvement in the following.2
- Assessment
- Call for help
- Positioning
- Suprapubic pressure
- Episiotomy assessment
- Internal rotation
- Delivery of posterior arm
Using a task trainer, students can focus on the fundamentals of building their confidence in performing specific skills and educators can measure and confirm that learners have mastered those skills. From here, learners can advance onto high-fidelity simulations or treat real patients, knowing they have the necessary foundational experience.
If your learners are in need of repetitive, isolated skills practice, a task trainer may be what you need to integrate into your training.
Standardized Patients – Improving Skills Performance for New Learners
The use of standardized patients (SP)s can be beneficial to develop a practitioner’s interpersonal communication skills. Because SPs can verbalize symptoms that they are experiencing, they are particularly useful in gathering patient history and diagnosing symptoms. By using a SP’s body language to convey certain information, healthcare professionals are required to be more observant of their patient.
One scenario developed by the University of Washington Medical Center Labor & Delivery Unit proved the benefits of using a SP in a birth scenario. Enacting an obstetrical bleeding emergency, the SP provided critical triggers to the healthcare team. As the patient’s condition worsened, the SP became anxious and concerned.3 By using this type of practice, learners improved their observational and professional skills.
By incorporating a SP into your scenario, you can introduce a real, human element to your simulation training. Learners can converse with a "real" patient, observing physical cues and considering their overall demeanor to form a more complete diagnosis.
Combining the Two – Hybrid Simulation Offers the Best of Both Worlds
Task trainers and SPs share one key benefit: they both can be included in your simulations in creative ways. You are free to be as imaginative as you'd like – especially if you consider hybrid simulation as an option. Hybrid simulation is when two or more simulation modalities are used in the same simulation session (i.e. attaching a task trainer to a SP). Using this form of simulation can allow for an integrated practice of both technical and communication skills.4
Research shows that learners have more engaging patient interactions with a SP but are likely to use a realistic, procedural touch more frequently with manikins.4 Hybrid simulation is one means to improve both clinical treatment and a learner’s patient interaction skills.
By combining the two forms of simulation in one scenario, you can effectively teach the complexities associated with birth, while also helping learners develop their communication and rapport with a patient.
Simulation is Never a One-size-fits-all Solution
Taking into consideration a program’s size, budget, and learning goals, each simulation should be and will be different. For scenarios that do not require high-fidelity, resource-rich simulation equipment, there are other options available.
Whether they are used together or alone, task trainers and standardized patients both have their unique role. They can enforce foundational clinical assessment and procedural skills and help to develop a learner’s interpersonal and communication skills, respectively. What is even more exciting is that, when used appropriately together, they can help you achieve both skill sets in your learners.
Read more about the solutions Laerdal offers

Want more content like this?
Sign up for Laerdal Medical email updates. You can identify your interests and receive new educational content, updates, event information and more.
References
- Le Morvan, P. & Stock, B. (2005). Medical learning curves and the Kantian ideal. Journal of Medical Ethics, 31(9); 513-518.
- Fialkow, M.F., Adams, C.R., Carranza, L., Golden, S.J., Benedetti, T.J., & Fernandez, R. (2014). An in situ standardized patient based simulation to train postpartum hemorrhage and team skills on a labor and delivery unit. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 9(1): 65-71. doi:10.1097/SIH.0000000000000007
- Flynn, K. (2012). The use of standardized patients to minimize anxiety in undergraduate nursing students in the clinical setting. Retrieved from http://sophia.stkate.edu/cgi/viewcontent.cgi?article=1057&context=ma_nursing
- Lopreiato, J.O. (2016). Healthcare simulation: Dictionary. Rockville, MD: Agency for Healthcare Research and Quality
- Coffey, F. Tsuchiya, K., Timmons, S., Baxendale, B., Adolph, S., & Atkins, S. (2016). Simulated patients versus manikins in acute-care scenarios. Clin Teach, 13(4): 257-61. doi: 10.1111/tct.12425