How Simulation Can Uncover Latent Safety Threats
Simulation can be a powerful method for amplifying your patient safety efforts in this area.

Simulation can be a powerful method for amplifying your patient safety efforts in this area.

Dr. Victoria Brazil, emergency physician and educator1
Are you confident in your hospital’s current approach to identifying and mitigating latent safety threats (LSTs) in your system to improve patient safety?
Latent safety threats (LSTs) are often referred to as “accidents waiting to happen.”2 LSTs are system issues that aren’t immediately apparent and can make it easier for healthcare providers to make errors.3
There is increasing recognition of the use of in situ simulation, or simulation that occurs in the real healthcare environment, as a powerful quality improvement tool for uncovering LSTs.5
Read on to explore how you can use in situ simulation to help uncover LSTs and drive quality improvement in your hospital.

Because it takes place in the actual clinical setting, in situ simulation can lend a unique opportunity to uncover LSTs involving your own equipment, space, processes, and protocols before they ever reach a patient.
Dr. Andrew Petrosoniak, MD, MSc (Med Ed), FRCPC, Emergency Physician and Trauma Team Leader at St. Michael’s Hospital in Toronto, Canada, compares in situ simulation to crash testing a car.6 "You can imagine that no car company is ever going roll out a car that hasn’t been crash tested," he points out. "It's not sufficient to just drive it around the neighborhood and say that it’s safe. It needs to be put through a collision. In simulation, it’s the exact same process. We can replicate systems, processes, [and] we can study physical spaces much better using simulation and understand exactly how things will work before a patient ever arrives."
Below, we discuss 5 types of LSTs that simulation has helped uncover along with some tangible examples of how hospitals have leveraged this powerful tool to elevate their patient safety efforts.

Patient safety experts agree that communication and teamwork are a crucial component of safe, effective patient care.7 But communication breakdowns are the leading factor contributing to sentinel events.8
In situ simulation provides a risk-free environment for assessing and improving team dynamics and communication. Simulations can replicate multi-disciplinary scenarios that involve interactions among various healthcare professionals, including physicians, nurses, pharmacists, and other team members. A well-designed simulation scenario followed by a careful debriefing can identify LSTs related to miscommunication, misunderstandings, or breakdowns in communication among different members of the healthcare team.
When you think about the types of scenarios in which solid teamwork is of the utmost importance, codes may come to mind. A study of trauma resuscitation using in situ simulation team training found 843 LSTs during 12 simulations.9 Fifty percent of them involved teamwork and communication, and many of the LSTs were categorized as critical threats.
LSTs included:
The shared mental model, or "getting everyone on the same page," is well-known as an important element of successful teamwork and collaboration in healthcare.10
Simulation has been found to help develop shared mental models in interprofessional healthcare teams.11 After participating in simulations at Cincinnati Children's Hospital Medical Center, the team found that developing a shared mental model was so crucial that the frontline nurses insisted it be added to their resuscitation flow sheet as a component that must be communicated with the team within the first 3-5 minutes of caring for a critically ill patient.12
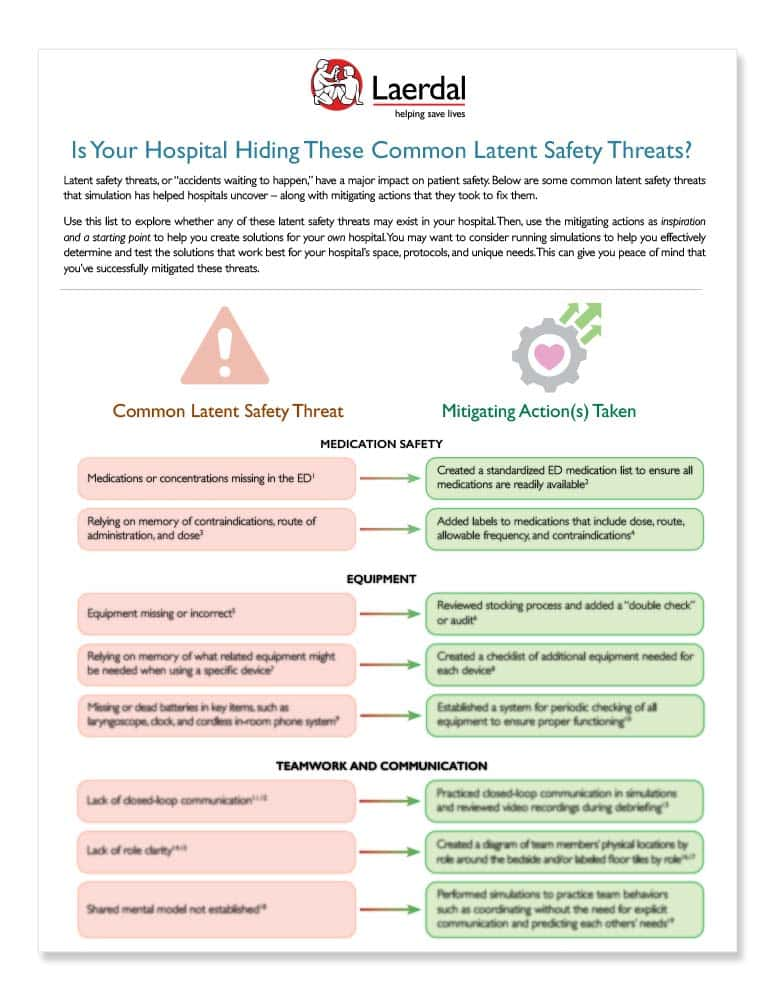
Download this checklist of common LSTs and how organizations have solved them, so that you can explore these areas in your own organization.

In situ simulation can successfully identify common staff knowledge gaps throughout every step of a scenario. For example, by running a single code scenario, you can identify knowledge gaps from appropriate dosing of epinephrine, to performing high-quality CPR, to operating equipment like the defibrillator correctly.
Because codes are low-frequency emergencies, maintaining currency of skills can be a challenge – but it can have major implications in the face of a cardiac arrest. At Boys Town National Research Hospital in Boys Town, NE, simulation helped them uncover a knowledge gap with their defibrillators. They had purchased new defibrillators in 2021 – but because the new defibrillators had never been used, the staff’s competency was no longer up to date. Uncovering the knowledge gap allowed them to take corrective action and ensure staff were proficient before a real cardiac emergency. This was just one of countless LSTs they uncovered through simulations.
A New York City hospital conducted 74 code simulations.13 They noted 29 instances of knowledge gaps in how to operate the defibrillator – including how to turn it on, utilizing AED mode vs. manual mode, use of CPR feedback mechanism, and pad placement. Since this discovery, they’ve added debriefing teaching points to simulations to reinforce knowledge of the defibrillator after every simulation and are also conducting more defibrillator training and review in their simulation center.

Simulation scenarios allow healthcare professionals to practice the entire process of medication administration, from prescription to dispensing and administration to the patient.
Common medication LSTs that simulation has identified include:
The Pediatric ED at the Cincinnati Children’s Hospital Medical Center conducted 90 in situ simulations.14 They discovered 73 LSTs – and 30% of them were related to medication safety, including:
Another multi-center study consisting of simulations of obstetric emergencies found issues with:15
In all of these examples, simulation allowed these hospitals to put corrective measures in place before they ever reached a real patient.
Dr. Andrew Petrosoniak shared how his hospital used simulation to drastically improve their massive transfusion protocol.16
They uncovered issues including:
They streamlined their process to order blood and educated the porters on the crucial nature of receiving blood rapidly for a trauma patient. When they later measured how their protocol adjustments were translating to actual patient care, they found some amazing results:
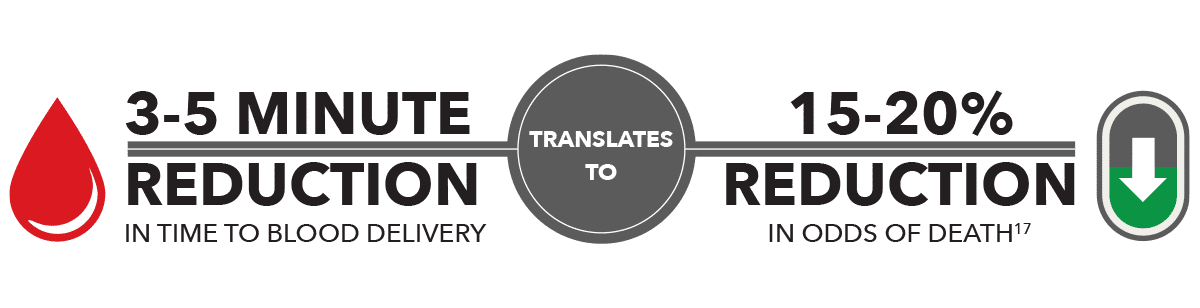
This example illustrates that utilizing simulation to expose and improve protocol issues can make a substantial impact on patient care.

One of the greatest benefits of in situ simulation is that it allows you to use your own equipment. In doing this, many hospitals have found issues with:
![]()
Not knowing the location of equipment, resulting in delays to care
![]()
Not having equipment organized in a specific area
![]()
Equipment not working
![]()
Equipment missing
In one study consisting of 18 in situ simulations performed across 11 EDs, they uncovered a total of 158 LSTs - 25% of which were related to equipment,18 including:
![]()
Equipment not easily accessible, including central line and chest tube
![]()
Equipment failure, including a failing laryngoscopy light and transvenous pacer balloon
![]()
Non-appropriate equipment identified, including equipment that was out-of-date
Simulations can also be tailored to include medical equipment malfunctions. This allows healthcare professionals to practice their response to such situations, identifying LSTs related to equipment reliability, maintenance issues, and potential consequences for patient care.

A number of studies show a connection between a positive safety culture (one in which safety is a shared priority) and improved patient safety.19
In situ simulation can help you promote a culture of safety by showing your teams that they can play a critical part in improving the system – and empowering them with the knowledge that they can make a real impact on patient outcomes in your hospital.
Download this checklist of common LSTs and how organizations have solved them, so that you can explore these areas in your own organization.