3 Ways High-Fidelity Simulation Can Improve NICU Performance


If you're a professional providing neonatal care, you understand how critical and time-sensitive emergencies can be. But because these events occur at a low frequency, opportunities for repetitive practice and experience are limited.
High-fidelity simulation can create realistic scenarios that mimic the realities of these critical situations without posing any risk to real patients – including the smallest, most vulnerable ones. It provides a safe, consistent, and standardized opportunity for NICU teams to train for optimal performance and ultimately improve clinical outcomes for newborns.
Regular simulation training of neonatal emergencies has been shown to positively impact patient safety.4
Below, we explore 3 areas where simulation can make a profound and positive impact in your NICU.

The extreme time-critical nature of neonatal resuscitation emergencies demands that caregivers be competent, confident, and ready to work together to respond optimally.
Neonatal morbidity increases by 16% for every 30 seconds of delayed initiation of positive pressure ventilation (PPV).5
But some data from real-life cases on the timeline of events suggest that major resuscitation events such as intubation, umbilical venous catheter (UVC), endotracheal (ETT), and intravenous epinephrine are often significantly delayed.6
Research shows that the infrequency of resuscitation events, the lack of repetition, and inexperience leave many caregivers feeling unprepared.7 Resuscitations can be compromised by cognitive and task overload, as well as inefficient communication and teamwork.8
Neonatal resuscitation certification typically occurs every 2 years. However, research suggests that skill retention starts to decrease just 3 to 8 months after training if the skills are not regularly practiced.9
Quality improvement efforts are essential to keep up with the clinical knowledge and skills that may decline over time.10 Continued simulation-based practice helps healthcare providers maintain strong, long-term performance between recertification periods.
By providing regular and diverse simulation training experiences, you can ensure that learners remain confident in their ability to address any neonatal emergency.
Resuscitation isn’t the only area that simulation can help. High-fidelity simulation can build preparedness in a wide range of low-frequency, high-frequency scenarios, including those noted among the leading causes of neonatal mortality:
A preterm baby simulator with accurate anatomy and functionality, as well as realistic facial and skin features, can bring scenarios to life. This can help elicit caregivers’ emotions in a way that makes training especially effective.

The transition from academia to the workforce is a difficult and often overwhelming time for new graduates. Research shows that new graduate nurses are linked to patient safety issues, such as near misses, adverse events, and practice errors.11
The transition to practice is such a major issue that independent healthcare patient safety expert ECRI listed “Challenges Transitioning Newly-Trained Clinicians from Education to Practice” as the #1 patient safety concern for 2024.12
According to ECRI, 30% of new nurses report that they don’t feel well-prepared to practice on their own.13 And, survey data suggests that there is reduced mindfulness around the culture of safety among new caregivers who’ve been in practice for less than a year.14
Research on new graduates in the NICU found that new grads experience a different and more complicated transition to practice compared to other areas of the hospital.15
Simulation has been shown to increase competence in new nurse graduates.16 It reduces their anxiety and increases their ability to think critically instead of becoming scared and flustered in high-stakes situations17 like those encountered in the NICU.
A 2024 study found that high-fidelity simulation of neonatal Crisis Resource Management events significantly enhanced newer NICU nurses’ confidence in their skills.18
Simulation can help you give new clinicians the practice they need to work competently and confidently in your NICU.
Over 5,000 healthcare institutions and systems worldwide rely on ECRI to guide their patient safety initiatives.19 ECRI recommends taking a total systems safety approach to design a strong safety and clinical operating system that recognizes and mitigates the risks associated with inexperienced clinicians.20
In situ simulation, or simulation that occurs in the real healthcare environment, can serve as a powerful quality improvement tool for uncovering and mitigating threats associated with transitioning new caregivers to the NICU. Because it takes place in the actual clinical setting, in situ simulation can lend a unique opportunity to bring everyone together to uncover issues involving your own equipment, space, processes, and protocols before they ever reach a patient.
In situ simulation can also help you promote a culture of safety by showing both new and tenured caregivers that they can play a critical part in improving the system – and empowering them with the knowledge that they can make a real impact on patient outcomes in your NICU.
A tetherless full-term and/or premature baby simulator designed specifically for in situ simulation adds considerable ease, mobility, and efficiency with setup by eliminating the need for cable connections.

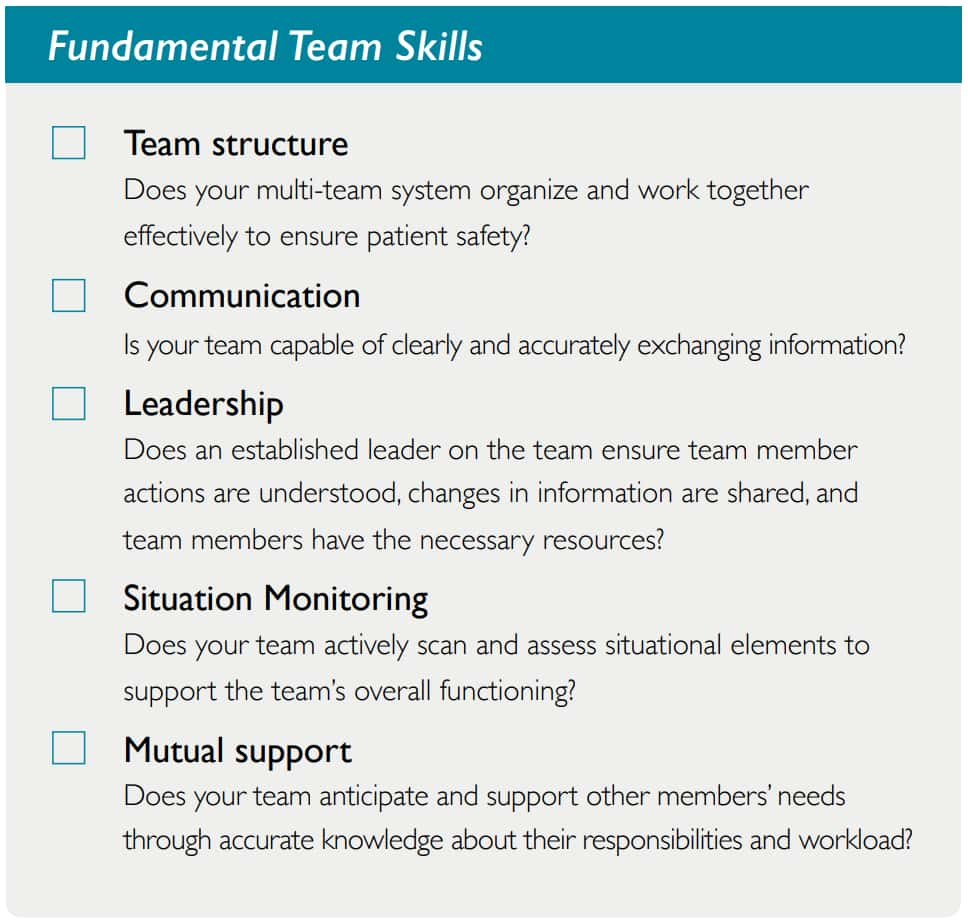
Effective interprofessional teamwork is especially crucial in the NICU.21 Human factors and non-technical skills such as leadership, communication, and collaboration are crucial in improving team performance and preventing medical errors.22
There’s a common assumption in healthcare that clinical competence naturally leads to strong communication and teamwork. That’s not the reality, though.
Research indicates that 30% of errors reported in the NICU stem from communication and teamwork interactions.23
Ineffective teamwork is a root cause of 30% of resuscitation procedures being performed improperly or not performed at all by resuscitation teams.24
Simulation has evolved over the years to become an essential tool for team training.25 And, it’s increasingly being used in quality improvement (QI) initiatives and to enhance safety culture.26
Simulation provides a risk-free environment for assessing and improving team dynamics and communication. A well-designed simulation scenario followed by a careful debriefing can identify issues in miscommunication, misunderstandings, or breakdowns in communication among different members of the healthcare team.
Simulation has been shown to improve interprofessional education, increase collaboration, and give caregivers deeper insight into other’s roles.27
A 2024 study looked at the effectiveness of simulation-based interprofessional education (IPE) on teamwork and communication skills in neonatal resuscitation. After participating in the simulation-based IPE program, the resuscitation team’s teamwork, communication skills, and clinical performance significantly improved. The participants’ clinical judgment skills and interprofessional attitude also improved, and they showed high education satisfaction.28
The study concluded that “repetitive training could help ensure more accurate neonatal resuscitations, ultimately contribute to the reduction of mortality rate from asphyxia, and enhance the quality of care.”29
A 2023 study looked at the impact of simulation on multidisciplinary NICU teamwork during delivery and transport of extremely preterm infants. Seven teams (each including one NICU fellow, two NICU nurses, and one respiratory therapist) participated in three high-fidelity simulation scenarios. The high-fidelity teamwork-based simulation curriculum decreased time to complete key clinical tasks in the resuscitation and transport of extremely preterm infants.30
Dr. Lou Halamek,
Professor of Neonatal and Developmental Medicine
Department of Pediatrics at the Stanford University School of Medicine

If you’re interested in using simulation-based training to improve performance and patient outcomes in your NICU, Laerdal can help.
Our mission at Laerdal is Helping Save Lives. One of the ways we pursue that mission is to ensure that clients can use simulation-based training and education to prepare their staff to deliver the best possible patient outcomes. Our goal is to help save an additional 1 million lives annually by 2030.
Contact your Laerdal representative today so we can begin a discussion on how we can best support you.
