3 Key Highlights of the AHA 2020 Guidelines
Catch up on some changes you may have missed during the pandemic and explore ways to train for them.

Catch up on some changes you may have missed during the pandemic and explore ways to train for them.

Since the first American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care (ECC) were published in 1966, the healthcare community has continually turned to the AHA for the latest resuscitation science and recommendations available.
If you’re an educator in resuscitation, you likely know the significance of the Guidelines and the importance of reading them in their entirety. But if you’re like many of our clients, you may have struggled to focus on the current Guidelines published last year – because they were released in October, in the midst of the COVID-19 pandemic.
Below, we summarize three new Guidelines recommendations that have our clients talking. We’ve also provided some suggestions for how to train for these recommendations based on the Resuscitation Education Science section of the 2020 Guidelines.
The intravenous (IV) route has historically been the primary method of vascular access during resuscitation. However, it can be difficult to secure an IV, depending on the patient’s condition and experience of the practitioner. This difficulty can lead to delay in administering drugs or fluids to the patient.1
The intraosseous (IO) access method is an alternative to IV that has grown in popularity and is often used as a first-line approach to access because many providers find it quicker and easier to accomplish.2 The previous 2015 AHA Guidelines did not make a recommendation for one method over the other.3
AHA’s new recommendations are that it is reasonable for providers to first attempt establishing IV access, and IO access may be considered if attempts at IV access are unsuccessful or not feasible.4

Resusci Anne QCPR with IV arm
Training tip:
IV insertion can be daunting and challenging for learners. Consider adopting components of the deliberate practice and mastery learning model to help learners perfect this psychomotor skill. Deliberate practice involves giving learners a distinct goal to accomplish; immediate feedback on their performance; and plenty of time for repetition to improve performance. Mastery learning involves using deliberate practice along with testing that uses set criteria to define a specific passing standard that implies mastery of the task being learned.5
AHA recommends combining repetition with individualized feedback based on assessments; assigning specific exercises to address areas for improvement; and providing learners with enough time to achieve the minimum passing standard.6
Paired with an IV arm task trainer or manikin with IV arm, this approach can help raise learner competence to an expert level.
Why:
According to the Resuscitation Education Science section of the 2020 Guidelines, incorporating a deliberate practice and mastery learning model may be considered for improving skill acquisition and performance.7 Evidence indicates that the model improves multiple learning outcomes when incorporated as part of BLS or ACLS courses.8

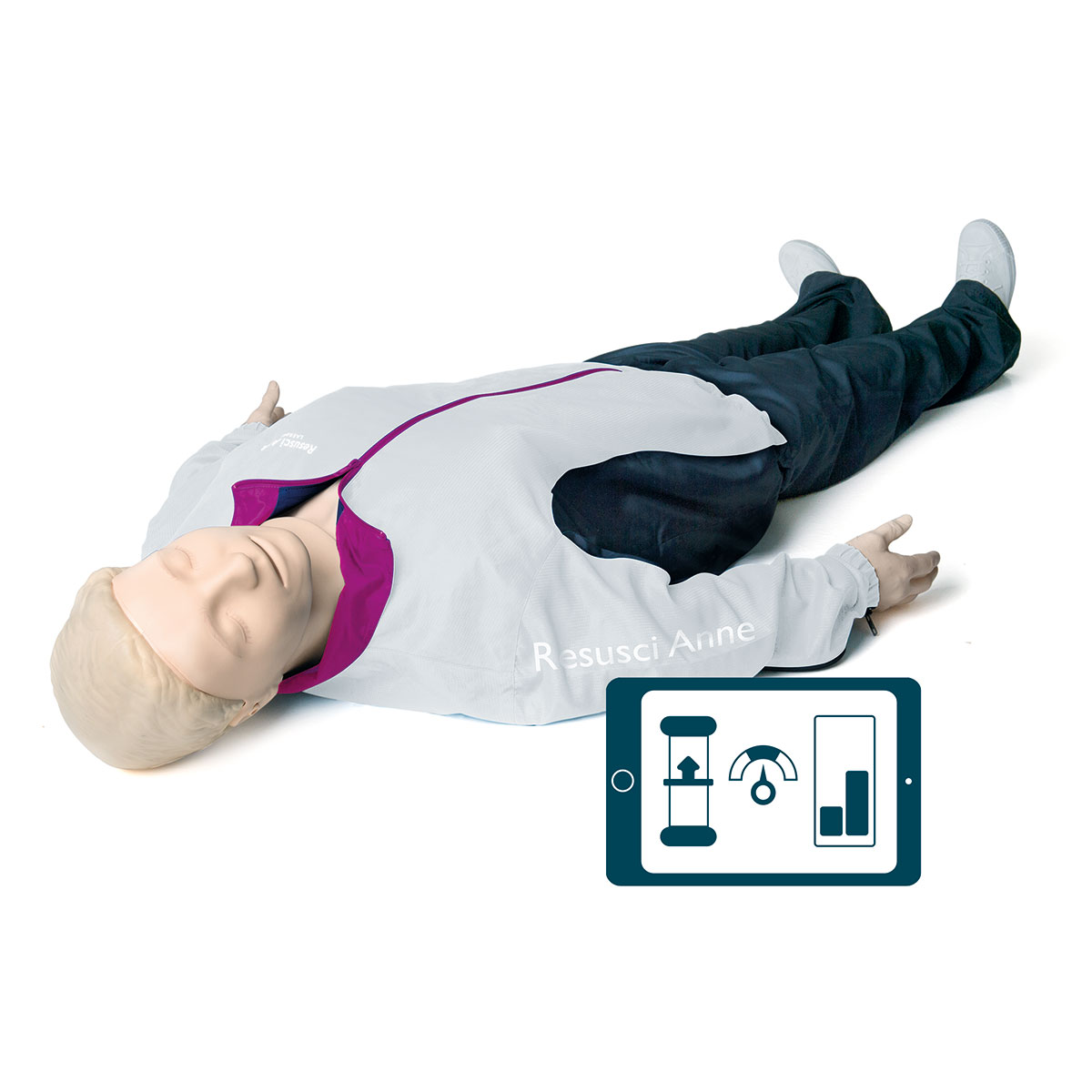
Resusci Anne QCPR with TeamReporter app
Double sequential defibrillation, or applying shocks nearly simultaneously using 2 debrillators, has become an increasingly popular approach. The technique is based on the idea that "more must be better."9
However, the Guidelines advise that the usefulness of double sequential defibrillation for refractory shockable rhythms has not been established. Because evidence is lacking, it is premature for this method to be used in routine clinical practice.10
Given the unknowns around using the technique, consider focusing instead on a better-understood factor in defibrillation success: CPR quality. The quality of CPR performed prior to defibrillation has been shown to affect clinical outcomes.11 Specifically, longer pre-shock pauses and shallow chest compressions are associated with defibrillation failure.12 If high-quality CPR isn’t performed, double sequential defibrillation most likely will not make up for it.
Training tip:
Ensure your learners are contributing to the chances of achieving successful defibrillation. Run some drills and scenarios that require your learners to maximize time on the chest and perform quality compressions – in spite of whatever dynamics and variables the team encounters. This will provide the opportunity to practice individual skills as well as teamwork and communication. Consider gamifying these experiences with a competition: use CPR feedback technology to measure and score learners on their individual and team performance. Debriefing the experiences from start to finish will help identify areas for improvement.
Why:
According to the Resuscitation Education Science section of the 2020 Guidelines, teamwork training and gamified learning are opportunities to enhance resuscitation training and may improve learning outcomes.13 Studies that evaluated the effect of team and leadership training as part of ACLS training found a positive impact on provider skills during simulated and real cardiac arrests. Improvements were seen in 1 or more aspects of clinical task performance during simulated events – including time to initiation of CPR and defibrillation.14 Studies examining the effect of gamified learning showed an improvement in knowledge acquisition, knowledge retention, and CPR skills.15
AHA now recommends that it may be reasonable to use a respiratory rate of 1 breath every 2 to 3 seconds (20 to 30 breaths per minute) for infants and children who are either receiving CPR with an advanced airway in place or are receiving rescue breathing and have a pulse.16
As it is considerably higher than in previous Guidelines, this recommendation has spurred some concerns about overventilation among some members of the healthcare community.17 Many Medical Directors have reviewed their own protocols in light of the new AHA Guidelines and have ensured that their personnel are sufficiently notified about local policies going forward.

Resusci Junior QCPR with airway head
Training tip:
Regardless of your position on increased ventilations, it’s important to be reinforcing the message now. Few events are as stressful for providers as a pediatric patient experiencing a sudden cardiac arrest. In situ training, or training that occurs in the actual clinical environment, provides a more realistic experience. Running an in situ scenario can help learners feel more prepared by giving them the opportunity to practice the required ventilation rate in the same setting in which they’ll have to perform it. Consider using infant and child manikins that provide quality feedback, as well as tools to facilitate high-performance team training, to create a rich and well-rounded training opportunity.
Why:
According to the Resuscitation Education Science section of the 2020 Guidelines, it is reasonable to use in-situ simulation-based resuscitation education in addition to traditional training.18 Recent evidence indicates that when combined with other educational strategies, in-situ training has a positive impact on learning outcomes, performance change in the real clinical environment, and even patient outcomes.19
TeamReporter App
The mobile app designed for High-Performance CPR training with intelligent video debriefing.
Resusci Junior QCPR Airway Kit
A simple do-it-yourself upgrade kit for adding more advanced airway training capabilities to Resusci Junior QCPR.
SimPad PLUS with SkillReporter
QCPR feedback on a rugged, Laerdal-dedicated SimPad PLUS tablet. Additional features include CPR for Teams mode and ShockLink device connectivity.
SkillReporter app
Designed and built for healthcare responders, the SkillReporter app offers a new level of precision training for treating infants, children, and adults in cardiac arrest.