5 Examples of Quality Improvement in Healthcare
Real-Life Cases Using Simulation


Simulation is being used as a powerful tool for quality improvement in healthcare. This goes beyond training. Examples include helping teams identify system flaws, optimize processes, and improve patient safety. One of the most effective ways this is done is through in situ simulation, which takes place directly in the clinical environment where care is delivered.
In situ simulation offers a unique opportunity to practice for low frequency, high acuity emergencies, using your own space, equipment, processes, and protocols.
Through our Accelerate program, we work with hospitals every day as a quality improvement partner, supporting their efforts with in situ simulation. The experiences of hospitals like Pullman Regional Hospital, Boys Town National Research Hospital, and Bronson Health have offered valuable insights into how simulation can be a powerful engine for driving quality improvement.
Drawing from their Laerdal Accelerate journeys, below are five lessons learned about using simulation to drive healthcare quality improvement.
Available in North America, Laerdal’s Accelerate Program is an all-in-one solution that provides on-site simulation for targeted clinical scenarios by providing simulators, operators, facilitators, a curriculum, and teams/skills assessment.
With Laerdal Accelerate, we bring a sustainable, robust, and data-driven solution that is hassle-free for our clients. This frees them up to focus on training, skills assessment, and system evaluation without the distraction of equipment operation, setup, tear-down, administration, storage, logistics, or curriculum acquisition.

One of the most powerful benefits of simulation is its ability to capture objective, hospital-specific performance data. This data can be used to drive meaningful systems improvement in healthcare.
Pullman Regional Hospital, a small critical access facility, recognized the importance of preparing providers for emergencies they don't encounter every day, like Obstetrics (OB) complications.
- Jeannie Eylar, MSN
Chief Nursing Officer, Pullman Regional Hospital

They ran a postpartum hemorrhage simulation scenario. The simulation captured data on key actions, including the time it took to order and receive blood from the blood bank.
The drill revealed vulnerabilities in the time it took to get blood from the blood bank, which is an issue that exists in many hospitals.
Having objective data specific to their hospital gave them pathways to focus on in their Quality Assurance and Performance Improvement (QAPI) program.
Using the data, they were able to set goals, make improvements, and then simulate again to measure the effectiveness of the improvements.
The results were remarkable.
- Amber Roberts, MSN, RN
Hospital Education Coordinator, Pullman Regional Hospital

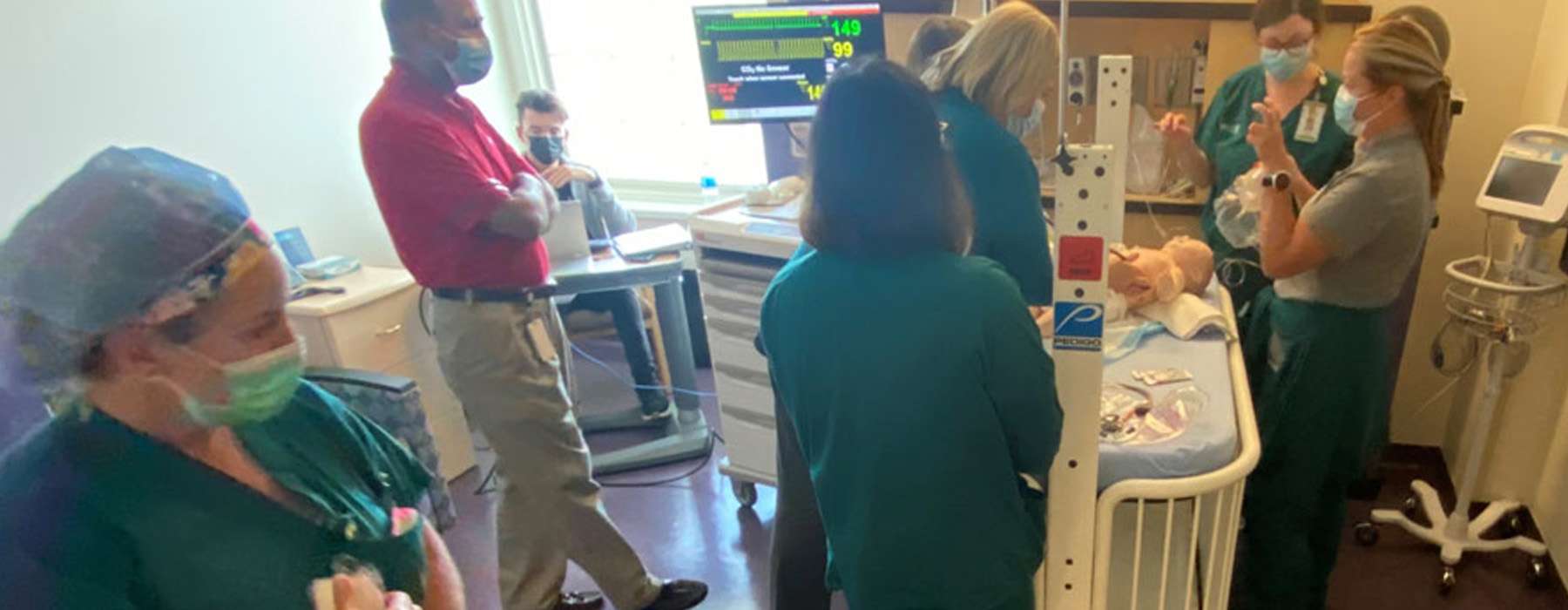
Improving patient safety is a collaborative effort. Simulation provides a safe, controlled environment to practice teamwork, communication, and coordination across multidisciplinary teams and departments without risk to patients.
At Boys Town National Research Hospital, one of the most important results of their simulation efforts was a significant improvement in teamwork. They found that the simulations helped “build bridges” and bring teams’ diverse experiences together to “speak a common language.”
- Dr. Mohan Mysore, M.D., FAAP, FCCM
Director of the Advanced Care Unit, Boys Town National Research Hospital
Post-event surveys of the participants confirmed the success of the simulations:
Confidence isn’t just an individual trait. It’s a shared resource that powers collective action. The most effective teams trust each other as much as their training, and this can markedly improve action at the patient bedside.
Boys Town National Research Hospital’s quality improvement in healthcare examples didn't stop at teamwork. In addition to using simulation to improve team performance, they also used it to uncover various latent safety threats – “accidents waiting to happen” – in the process. They were able to mitigate these issues before they ever affected a real patient.

Issue:
Simulation uncovered a knowledge gap on how to draw up Epinephrine with a 3-way stopcock.
Solution:
This is now reviewed and mastered during every simulation code scenario.
Issue:
Simulation uncovered a knowledge gap for when to call rapid response vs. code blue.
Solution:
Policy revisions have been made as to when and how to initiate which response and who responds to each.
Issue:
Simulation uncovered that re-education was needed on new defibrillators that had been purchased in 2021 but had never been used in an actual emergency.
Solution:
This is now reviewed in simulation scenarios and during annual competency checks.
Issue:
A Local Anesthetic Systemic Toxicity (LAST) simulation scenario for OR/PACU uncovered a need for a policy/protocol.
Solution:
The PACU team has since developed a new LAST policy/protocol.

- Andrew Petrosoniak, MD, MSc (Med Ed), FRCPC
Emergency Physician and Trauma Team Leader at St. Michael’s Hospital in Toronto, Canada
Carol Fuller, RN, BSN, MBA, C-EFM, CENP, C-ONSQ, is the former System Director of Nursing for Women and Children’s Services at Bronson Health. She was committed to ensuring that every pregnant patient has a safe birth. With that goal in mind, she worked with her Risk Management department and an outside consultant to perform risk assessments of all OB services.
One of the identified risks was the limited time to practice emergency clinical procedures as a team and test current processes. They decided to turn to simulation to test how well everything was working. They simulated both postpartum hemorrhage and eclampsia.
The eclampsia simulation scenario generated key data insights on actions taken in areas like:
including requesting anesthesia assistance and suction apparatus
including administration of antihypertensive and magnesium sulfate
including correctly ordering and administering antihypertensive and magnesium sulfate bolus
including assessing patient orientation and checking external fetal monitor
- Carol A. Fuller, RN, BSN, MBA, C-EFM, CENP, C-ONSQ
Former System Director of Nursing for Women and Children’s Services at Bronson Methodist and Bronson Battle Creek Hospital

Afterward, Carol and the leadership team had the opportunity to review the data collected during the simulation. Not only did it provide insight into a few key areas of opportunity, but it also highlighted areas of success for the team to be congratulated and encouraged to keep going.
“The providers really like the data because they’re very data-driven," she says. "It also gave us opportunities to look at where we need to focus.”
Our experience with Bronson Health, and with every other client, is that awareness is the first step toward change – and with data in hand, that change becomes actionable.

Perhaps one of the most meaningful quality improvement examples in healthcare using simulation occurred at Bronson Health. Their efforts started to pay off much sooner than they imagined.
One week after the simulations, a pregnant patient arrived one night via ambulance to the Emergency Department at Bronson Methodist Hospital. She had preeclampsia with severe features, very high blood pressure, and vision loss. Shortly upon arriving to labor and delivery, she had a seizure while already on magnesium – an unexpected and unusual clinical presentation.
But the staff had just simulated this exact scenario a week earlier, in labor and delivery. As a result, the clinical care team came together as a high-performance team to provide optimal care.
"Even though we’re a regional center, we really don’t see patients who seize while already on magnesium," Carol explains. “In the simulation, they went through this same scenario with this patient in the same situation. Then they ended up doing a second round with the real patient. It really helped them feel comfortable to get through all those steps."
“Everyone maintained their composure and moved the entire process along as fast as possible,” adds Dr. Paul Berkowitz, one of the Bronson Health Hospitalists who cared for the patient. “The nursing staff pulled together and performed as a well-oiled machine, taking fantastic care of this patient. Her care could not have been better once in our hands.”
Both mother and baby left the hospital a few days later with no lingering complications.
- Carol A. Fuller, RN, BSN, MBA, C-EFM, CENP, C-ONSQ
Former System Director of Nursing for Women and Children’s Services at Bronson Methodist and Bronson Battle Creek Hospital

"The simulation made a huge difference, even for my experienced nurses,” Carol says. “It could not have been more timely."
If you notice, none of the above stories are about better-training people. They are about improving teams and systems.
Data shows that in most organizations, 85% of quality issues are traceable to the system.2 And the above great healthcare organizations are using simulation to address that.
We’re doing some exciting things in the field of Healthcare Quality Improvement. Follow our Healthcare Quality Improvement hub page for more resources, and be sure to speak with one of our Laerdal representatives to see how we can help you in your efforts.
1. Petrosoniak, A. [@andrew-petrosoniak]. (2025, July 31). Why is it that in healthcare and across so many industries we often wait until an incident or near miss before making a change? [Post]. LinkedIn. https://www.linkedin.com/posts/andrew-petrosoniak_why-is-it-that-in-healthcare-and-across-activity-7331345925912625152-Hlsk/
2. Bova, T. (2023, July 11). 5 Factors That Make for a Great Employee Experience. Harvard Business Review. https://hbr.org/2023/07/5-factors-that-make-for-a-great-employee-experience