
3 New Products to Amplify Your Simulations
In situ Simulation
The training and education benefits of using simulation in a clinical environment have been proven across healthcare. Learners who participate in simulation training see improvements in retention, skills acquisition, and confidence compared to those who experience only didactic training.
In situ simulation creates even more learning-rich circumstances, giving learners an opportunity to practice complex scenarios in their real clinical environment. One study found that in situ simulation helped to identify latent safety threats (LSTs) in one hospital system. And, in situ simulation helped improve deliberate practice of teamwork, communication skills, and patient safety outcomes.1 With in situ simulation, team behaviors and system processes that might put a patient at risk can be uncovered and corrected before a real patient enters the room.
[Using in situ simulation] You can challenge the way students look at things and make mistakes in essentially a consequence-free environment.
Despite the growing body of evidence in support of simulation, there are areas often overlooked in terms of creating realism. In any given hospital, the variety of medical equipment is nearly incalculable. Depending on the unit, floor, or room, the most important and lifesaving equipment can be stored differently, operated differently, and require different training. There are likely multiple variants of the same type of equipment, purchased from different manufacturers or unique models purchased at different times. The time to discover that these variables can lead to risk is during a simulation -- not during an actual emergency.
In addition to identifying latent risk through in situ simulation, there is an opportunity to integrate existing medical equipment in your simulations. Doing this can lead to a positive impact on patient care. In this short article, we explain how introducing the use of real medical equipment in simulations can better prepare your learners to:
- Manage a ventilated patient
- Monitor a patient’s vital signs
- Perform defibrillation on victims of sudden cardiac arrest

Breathe Life into Your Simulation Environment
Managing a patient-ventilator interaction can be challenging, especially because of the complexity of today’s ventilators and the various ventilation modes. In situ simulation affords learners the opportunity to gain hands-on practice, which is made even more realistic when using a real ventilator.
For example, research has shown that acute respiratory distress syndrome (ARDS) is undertreated in terms of the use of recommended approaches to mechanical ventilation (MV). And, in-hospital mortality rate remains high.2 Additionally, there is little consistency among physicians when selecting ventilator settings to treat patients in ARDS cases.3 Simulation training with a ventilator allows learners to adjust the pressure accordingly and to interact as part of a whole – including voicing concerns to the rest of the medical team.
A study among anesthesiology residents proved that simulations using a simulator were more effective than solely computer-based simulation in terms of knowledge and skill acquisition related to MV.4 A firm understanding and implementation of lung-protective ventilation strategies has been shown to reduce mortality, and learners can achieve this level of competency through in situ training with a ventilator.

SimMan 3G supported by a ventilator with the help of the ASL 5000TM Lung Solution
To help you seamlessly integrate any ventilator into your scenario, we have introduced the new ASL 5000™ Lung Solution for the SimMan platform. Compatible with SimMan 3G, SimMan Essential, SimMan Essential Bleeding, and SimMan 3G Trauma, you can conduct training with a spontaneously breathing patient supported on a ventilator. With this practice, learners can develop the confidence and skill to manage a ventilated patient, while also acclimating to their real-world clinical environment.
Monitor Your Simulator the Same Way You Would a Patient
When a patient emergency occurs, the critical means for detecting, diagnosing, and treating the patient is to track the patient’s vital signs. Likewise, nurses monitor vital signs at regular intervals to confirm that the patient is stable. In the context of all the patient’s physiologic parameters, and under life-threatening conditions, continuous patient monitoring has proved to save lives.
The fact is that the patient monitor is a vital piece of equipment--one that nurses and doctors are trained to rely on as a matter of routine, especially in an emergency or ICU setting. During an in situ simulation, you can prepare nurses and doctors best by permitting them to see and rely on the patient monitor they will be using in real life.
One study of fourth-year medical students found that simulation-based learning aided the development of their critical assessment and management skills.5 This kind of training can lose its benefit, however, if learners are suddenly thrown a curve by experiencing details in real life that they did not experience in simulation. The detail of the correct patient monitor is an important one.
Even outside of the emergency department (ED) and intensive care unit (ICU) the benefits of using a real patient monitor are manifold—especially in an environment like MedSurg where patient monitoring can be more of a scheduled event and where alarm fatigue poses its own known issues. And, in this environment the benefits of improved clinical assessment skills are significant. Simulation not only helps to improve a clinician’s performance and ability to complete tasks, but also helps to reduce patient discomfort, complication rates, and costs of care.6
 VitalsBridge enables SimBaby to connect to a real patient monitor
VitalsBridge enables SimBaby to connect to a real patient monitor
VitalsBridge allows you to connect your own patient monitor to your simulator, providing an experience that more accurately parallels a real clinical experience in your facility. Learners can feel confident that their training has prepared them for the “real deal.” An increased level of comfort in evaluating vital signs can reduce the cognitive demand on a healthcare professional and can ultimately lead to a more rapid patient intervention.7
Find the Flaws in Your Defibrillation Before They Find You
In cases of sudden cardiac arrest (SCA), every second counts. When a patient codes, that is no time for a clinician to learn how to operate a particular defibrillator or to find out that it was not stored for easy access at the bedside. In situ simulation can provide the opportunity to discover and correct any flaws in the response system before harm occurs.
Simulation can elicit real responses from learners – responses they can learn from. It can also promote team engagement, and compliment existing quality assurance processes in hospitals.8 Experts suggest that simulation-based mock codes significantly correlate with improved SCA survival rates.9 These findings support that increased realism in simulations benefits both healthcare professionals and patients alike.
Team members on medical-surgical units need to be empowered with the knowledge and skill to avoid the classic trap: ‘The code team will do that when they arrive.’
To achieve this realism, we have developed SimMan ALS LiveShock. The combination of a SimMan ALS chest skin and an integrated ShockLink unit enables the use of a live defibrillator with real pads or paddles.
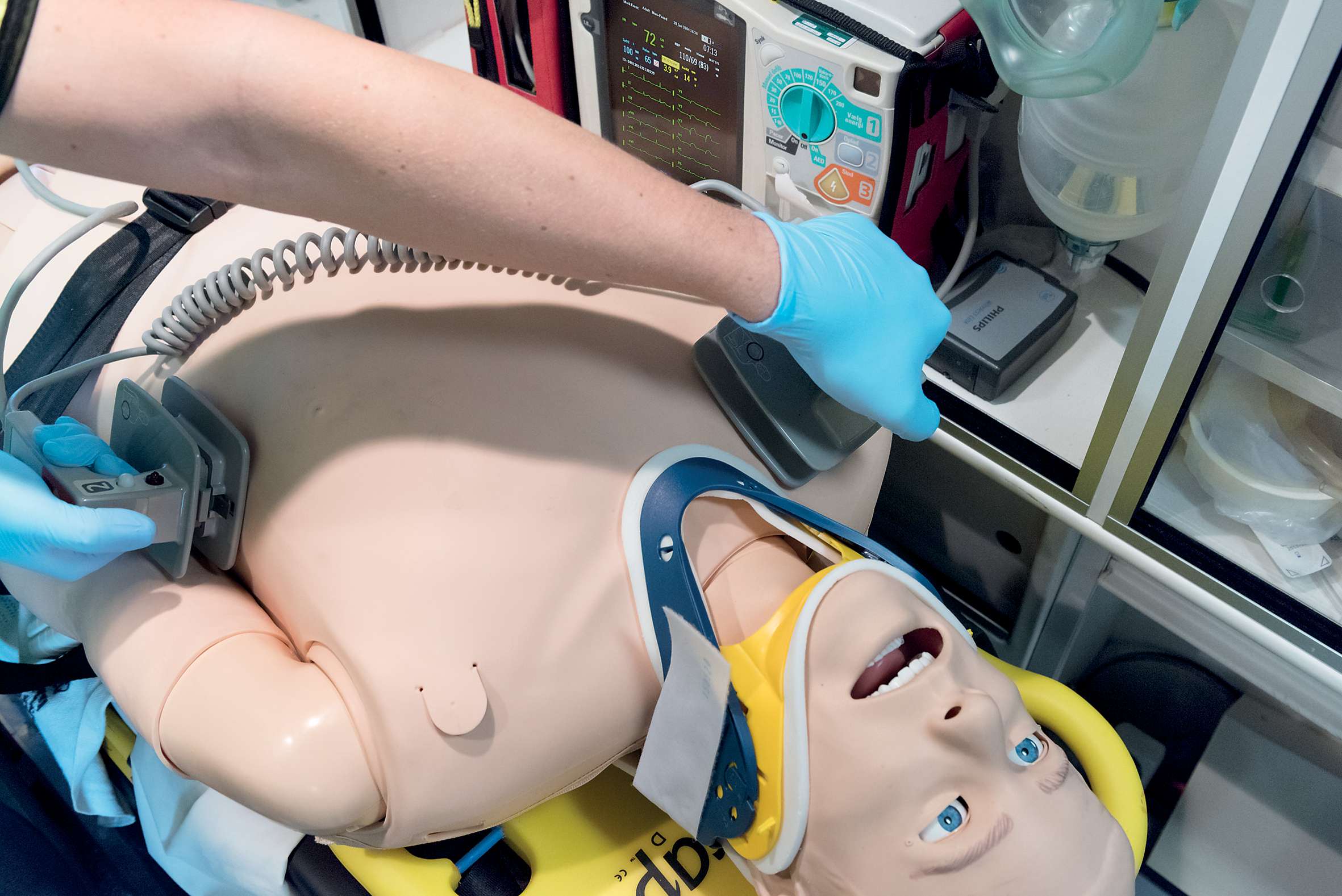 SimMan ALS LiveShock being shocked by a real defibrillator for a more authentic practice environment
SimMan ALS LiveShock being shocked by a real defibrillator for a more authentic practice environment
With the help of SimMan ALS LiveShock, your learners can practice resuscitating a patient with any available defibrillator at your facility. And, because you don’t need separate training pads or paddles, the learning experience can move along in real-time with no interruptions.
Improve Your In Situ Simulations With Added Realism
Learners cite increased confidence in their clinical environment and better knowledge acquisition after they have participated in a simulation.
In situ simulation is associated with a higher rate of skill application at the bedside.10
To augment the reality of your simulations, consider integrating your own medical equipment in the scenario. By doing this, your learners can gain exposure and familiarity with the equipment that will later help them to save lives.

Free "7 Tips for Effective In Situ Sim" Checklist
This checklist will help you measure your organization against best practices that others in simulation have come to rely on.
Helping You Succeed


References
- Patterson, M.D., Geis, G.L., Falcone, R.A., LeMaster, T., & Wears, R.L. (2013). In situ simulation: detection of safety threats and teamwork training in a high-risk emergency department. BMJ Quality & Safety, 22, p. 468-477. DOI: 10.1136/bmjqs-2012-000942
- Spadaro, S., Karbing, D.S., Fogagnolo, A., Ragazzi, R., Mojoli, F., Astolfi, L., et al. (2017). Simulation training for residents focused on mechanical ventilations. Simulation in Healthcare, 12(6), p. 349-355. DOI: 10.1097/SIH.0000000000000249
- Ibid
- Ibid
- Steadman, R.H., Coates, W.H., Huang, Y.M., Matevosian, R., Larmon, B.R., McCullough, L., et al. (2006). Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Critical Care Medicine, 34(1), p. 151-7. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16374169
- Gandhi, T. (2018). Include simulation in your improvement plans. Institute for Healthcare Improvement. Retrieved from http://www.ihi.org/communities/blogs/simulation-as-an-essential-element-in-learning-and-improvement
- Drews, F.A. (2008). Patient monitors in critical care: Lessons for improvement. Agency for Healthcare Research and Quality. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK43684/
- Lighthall, G.K., Poon, R., & Harrison, T.K. (2010). Using in situ simulation to improve in-hospital cardiopulmonary resuscitation. The Joint Commission Journal on Quality and Patient Safety, 26(5), p. 209-216. Retrieved from https://www.sciencedirect.com/science/article/pii/S155372501036034X
- Aebersold, M. & Tschannen, D. (2013). Simulation in nursing practice: The impact on patient care. The Online Journal of Issues in Nursing, 18(2). Retrieved from http://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-18-2013/No2-May-2013/Simulation-in-Nursing-Practice.html
- McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., & Scalese, R. J. (2010). A critical review of simulation-based medical education research: 2003–2009. Medical education, 44(1), 50-63.
*Cohen, E. R., Feinglass, J., Barsuk, J. H., Barnard, C., O’Donnell, A., McGaghie, W. C., & Wayne, D. B. (2010). Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simulation in Healthcare, 5(2), 98-102.
**Cason, M. (2017). Are your in situ simulations meaningful for all? NLN Center for Innovation in Simulation and Technology. Retrieved from https://nlnteq.org/2017/03/28/are-your-in-situ-simulations-meaningful-for-all/
