
Oppimisen kehä
Tuloksekas ja tehokas oppiminen perustuu selkeiden tavoitteiden asettamiseen. Jokaisessa oppimisen kehän viidessä vaiheessa tavoitteiden täytyy olla
- havaittavia
- mitattavia
- oppijakeskeisiä
- toimintapainotteisia.
The “see one, do one” approach to learning can be especially challenging for trainees in labor and delivery. Caring for two patients, the mother and the baby, creates double the possibility for complications and requires double the amount of patient monitoring. The learning curve in labor and delivery can be a never-ending one, and simulation is being used more often to prepare clinicians for low frequency, high risk events. Continuous practice helps staff recognize and potentially mitigate adverse events.1
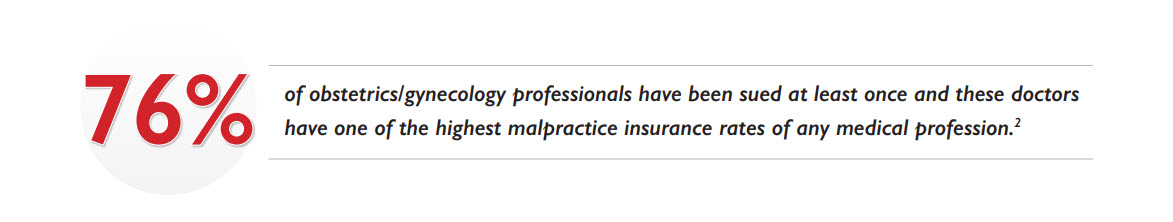
Risk is a major impetus for the use of simulation. Seventy-six percent of obstetrics/gynecology professionals have been sued at least once and they have one of the highest malpractice insurance rates of any medical profession.2 The most common clinical causes of medical litigation in obstetrics and gynecology are cases involving fetal distress, uterine rupture after a vaginal birth in a woman with a previous cesarean section, and shoulder dystocia.3
Consider that adverse obstetric events occur in approximately nine percent of all deliveries in the United States, and it is estimated that fifty percent of these events are preventable.4 It is no surprise that the Doctor’s Company, a national physician-owned medical malpractice insurer, advises using checklists and thorough documentation including care provided and the outcomes of care to reduce risk of litigation.5 They also recommend considering multidisciplinary simulation drills for maternal hemorrhage, respiratory arrest in mother and newborn, shoulder dystocia, placental abruptions, ruptured uterus, and other unexpected complications.Simulation practice can help to address risk and other concerns surrounding maternal care. The wide variety of simulation fidelity options (options for approximating reality) gives educators an array of tools to support experiential learning at all levels, from simple task trainers to sophisticated full-body manikins. This article examines the different advantages and limitations of using task trainers, standardized patients (SPs), hybrid simulation and manikins in various obstetrics and gynecology training situations. Each method can meet a particular need and amplify the learner’s competence within the different segments of the Circle of Learning. This cyclic, objectives-based tool provides context for planning and executing educational programs, with each segment addressing specific learner needs.
Simulation practice can help to address risk and other concerns surrounding maternal care. The wide variety of simulation fidelity options (options for approximating reality) gives educators an array of tools to support experiential learning at all levels, from simple task trainers to sophisticated full-body manikins. This article examines the different advantages and limitations of using task trainers, standardized patients (SPs), hybrid simulation and manikins in various obstetrics and gynecology training situations. Each method can meet a particular need and amplify the learner’s competence within the different segments of the Circle of Learning. This cyclic, objectives-based tool provides context for planning and executing educational programs, with each segment addressing specific learner needs.
Using a task trainer, students receive hands-on practice performing psychomotor skills independently and at their own pace. Typically, the focus will be on one specific task, such as pelvic exams, umbilical catheterization, or complicated deliveries.
Situations that require repeated practice are best suited for use of a task trainer. Learners are able to gain skills proficiency through supervised, tactile application. In a study evaluating the training of shoulder dystocia using a birthing simulator, learners saw a forty-four percent improvement in the mean scoring of their emergency procedure, including: 6
There was also a trend showing reduction in peak force used and a shorter delivery duration following the training. This is where “practice makes permanent” shows its true benefit. Wherever available, it’s worth considering use of a task trainer that can provide real-time assessment.
John’s Hopkins Medicine cites proper patient care as one primary benefit of task trainers.7 “It is understood that clinicians-in-training will treat patients; however, from an ethical perspective, harm to patients as a byproduct of training or lack of experience is justified only after maximizing approaches that do not put patients at risk”.8 Task trainers help by providing you with the ability to confirm that learners have, in fact, mastered a skill before allowing them to perform on real patients.
With less patient interaction and feedback, such as pain measurements and changes in vital signs, the use of a task trainer can be limited. Susan Galloway, a doctoral student in the Graduate School of Nursing at the Uniformed Services University of the Health Sciences in Bethesda, MD, stated that there is a “lower level of ability to suspend disbelief in a simulation scenario due to the single task purpose of the trainer”.9
At a lower price-point, task trainers in isolation may exponentially increase learner comprehension. If your learners require clinical attention to detail and hands-on, repetitive practice, a task trainer might be your saving grace.

Tuloksekas ja tehokas oppiminen perustuu selkeiden tavoitteiden asettamiseen. Jokaisessa oppimisen kehän viidessä vaiheessa tavoitteiden täytyy olla
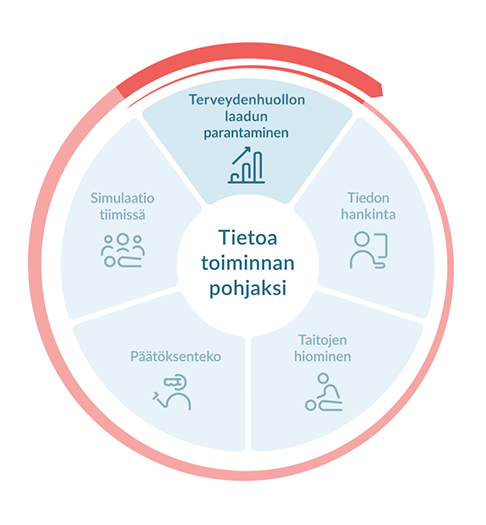
Oppijoille esitellään koulutustavoitteiden saavuttamiseen tarvittavat tiedot kirjojen, ammattijulkaisujen ja verkkosivustojen avulla. Tiedon hankintaa vahvistetaan itsearviointiprosessin avulla.
Tarvittaessa ohjaajilta voi kysyä lisätietoja ja he voivat arvioida oppimisen edistymistä.
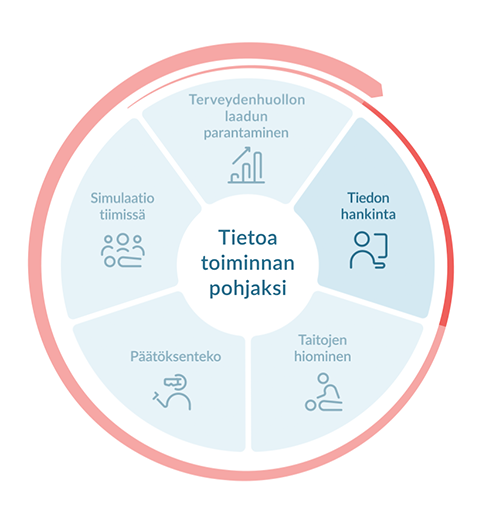
Tietojen hallitseminen on ehdottoman tärkeää parhaan hoidon tarjoamiseksi – huolimatta, siitä työskenteletkö yksin vai tiimissä. Opittuja taitoja on ylläpidettävä harjoittelemalla. Toistuva harjoittelu kouluttajien ja mallinukkien avulla tukee psykomotoristen taitojen kehittymistä. Jotkin taidot voidaan oppia yksilöllisesti käytännön harjoittelulla, mutta esimerkiksi ryhmätyö-, viestintä- ja johtamistaidot opitaan tiimeissä.
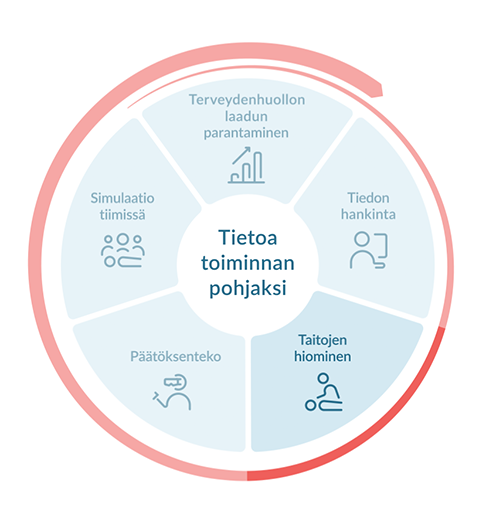
Interaktiivinen oikeiden potilastapausten simulointi ja siitä saatu palaute vahvistavat osaamiseen perustuvaa päätöksentekoa ja kehittävät kriittisen ajattelun taitoja. Tällainen itseohjattu oppiminen voi tapahtua missä ja milloin vain.
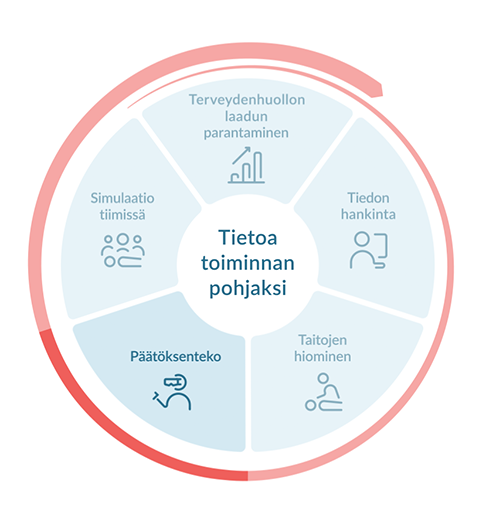
Hoitotyö on moniammatillista tiimityötä.
Tiimeissä harjoiteltavan simulaation avulla oppijat voivat harjoitella todellisen elämän skenaarioita realistisessa työskentely-ympäristössä ja pyrkiä siten hoitovirheiden vähentämiseen. Tämäntyyppisen koulutuksen avulla oppijat voivat parantaa tiimityöskentely-, viestintä- ja johtajuustaitojaan. Debriefing sekä yksilön että tiimin suoriutumisesta on ensiarvoisen tärkeää kehittymisen kannalta.
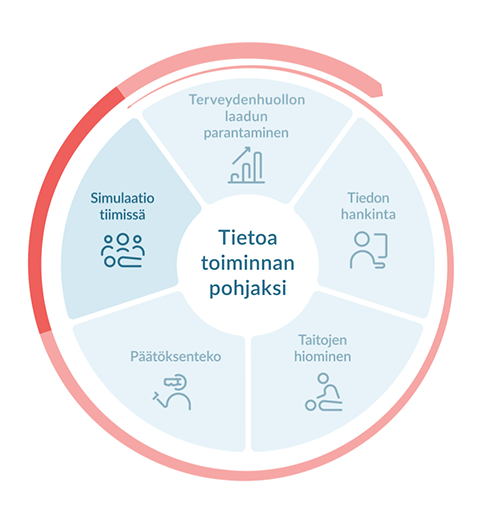
Oppiminen muiden toimintaa katselemalla ja seuraamalla on perinteinen koulutustapa, mutta oppiminen itse tekemällä on yhtä tärkeää. Kognitiivinen ja taitoihin perustuva oppiminen, joka on integroitu harjoitteluun, tukee terveydenhuollon ammattilaisten osaamisen kehitystä.
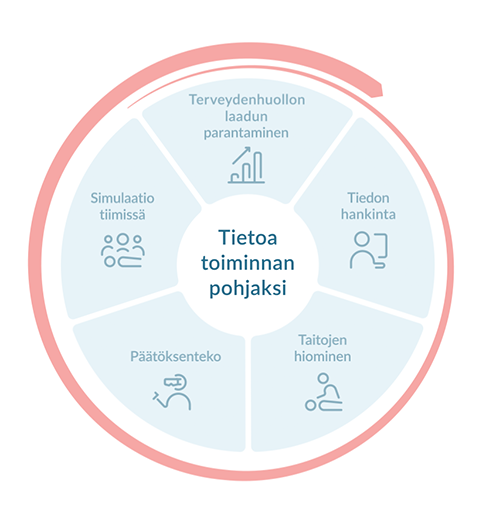
Nyt on mahdollista kerätä ja analysoida tietoja käyttäytymisestä ja suorituskyvystä oppimissyklin jokaisessa vaiheessa. Tätä näkemystä voidaan käyttää annettaessa palautetta yksittäiselle oppijalle, ryhmille, ohjaajille ja koulutusadministraattoreille. Suorituskyvyn parantamiseen liittyvien ehdotusten lisääminen tuo tietoa toiminnan tueksi ja parantamiseksi.
Realistically portraying a scenario, SPs interact with learners to create a low-risk, reduced-stress learning experience. Because SPs are able to verbalize symptoms and communicate what they are physically experiencing, they can be useful in gathering patient history and diagnosing symptoms. For example, a female SP can state that she has pain in her abdomen, followed by blurred vision and fainting, which may indicate pre-eclampsia. There is also opportunity for SPs to play the part of family members, providing history about the patient while adding realism to the scenario.
Additionally, learners can read the SP’s body language and incorporate that information into their clinical assessments. One scenario was developed by the University of Washington Medical Center Labor and Delivery Unit to represent an obstetrical bleeding emergency. A standardized patient was used to provide critical triggers and prompts to the team; as the scenario progressed and the patient’s condition worsened, the female SP became more anxious and concerned with her clinical status.10 Learners can use this type of interactive practice to improve their observational and relational skills.
SPs allow learners to practice communication skills, establishing what questions need to be asked or how to relay bad news. Allowing the opportunity to recall didactic lessons and put acquired knowledge into action may lead to higher levels of engagement and self-awareness for learners.
There are some important factors to assess when considering the use of a standardized patient: 11
Through the use of a SP, learners gain clinical experience while practicing patient-centered and respectful care in a low-risk environment. Rehearsing patient interactions with a “real” patient can make the simulation come to life and allow for fine-tuning of interpersonal and professional skills. If you are interested in facilitating an engaging learning process, using a standardized patient may be a great place to start.
Simulation can be as creative as the educator and the learners allow. Hybrid simulation is when two or more simulation modalities are used in the same simulation session. Typically, a task trainer or partial simulator is realistically affixed to a SP, allowing for teaching and assessment of technical and communication skills in an integrated fashion.12
According to a recent study, learners had increased interactions with standardized patients compared to manikins, and their behaviors were more akin to what one would expect in real, clinical practice. However, they were inclined to use procedural touch more frequently with manikins, lending more effective hands-on training. 13 Hybrid simulation combines both forms of practice for learners – communications and clinical treatment.
The use of a SP and birthing simulator may be able to effectively teach the complexities associated with birth, while ensuring that learners communicate and monitor the patient as well. The interaction with a “real” patient combined with hands-on clinical practice can reinforce competent decision making and develop critical thinking skills. Learners can then apply these skills to actual patient encounters, confidently ascertaining the best course of treatment.
It puts you closer to a real-life situation – need more of it!
Actors made the simulation more realistic and required you to think critically
The delivery progressed more naturally and hands-on experience is always better than lecture
It gets you thinking more about real-life experience...
Hybrid simulation offers a bridge between simulation methods in that learners can work with a real patient and perform clinical skills. Even so, it can be limited by the technology of the task trainer or simulator in use. Similarly, facilitating a hybrid simulation includes both training a SP and setting up the task trainer or simulator. Even partial simulators can be high-fidelity and preparing for a simulation session can include scenario preparation and maintenance.
Hybrid simulation deserves attention when determining how to reinforce your learning objectives. It offers interpersonal and palpable practice for your learners. To help learners develop their decision-making competency, you may want to consider expanding your simulations to incorporate both standardized patients and task trainers.
It is understood that cliniciansin-training will treat patients; however, from an ethical perspective, harm to patients as a byproduct of training or lack of experience is justified only after maximizing approaches that do not put patients at risk.10
Today’s technologically advanced manikins and accompanying systems offer an unprecedented level of fidelity. They provide a valuable means for educating interdisciplinary teams–developing their knowledge and clinical skills while protecting patients from unnecessary risk.
Simulators are particularly well-suited for simulations involving traumatic or emergency scenarios. Obstetrics is a key area where manikins have been instrumental in simulating emergencies during labor and delivery. Due to the nature of the emergencies and patient age, educators count on manikins to provide a realistic physiology where SPs cannot.15
In addition, team dynamics are critical when faced with an emergency situation. Dr. Salvatore Politi, an Associate Professor in Radiology at University of Massachusetts Medical School, states, “A formalized activation system, good leadership, and good organization of team members, with each member well trained in the management of obstetric emergencies, helps facilitate a smooth delivery of the fetus”. 16 He also recommends, “Despite its infrequent occurrence, all healthcare providers attending pregnancies must be prepared with a high level of awareness and training to handle vaginal deliveries complicated by shoulder dystocia”.17 One solution can be simulation with a simulator, which can provide learners with the ability to practice simulation in teams, reacting to physiological changes in real time, and rehearsing real world scenarios.
The capability for weighing and enacting a clinical pathway is one thing that other methods of simulation cannot deliver. Use of a simulator allows for administration of medication and physiological monitoring, so that learners can grasp the reality of their actions. Additionally, scenarios allow for evidence-based decision making, using clinical procedure in tandem with real human factors and behaviors. As scenarios follow the same treatment logic as an actual case, the patient will respond according to the clinical interventions taken. This becomes especially important when training for situations as complex as labor and delivery emergencies.
A formalized activation system, good leadership, and good organization of team members, with each member well trained in the management of obstetric emergencies, helps facilitate a smooth delivery of the fetus.16
At Laerdal, our clients appreciate when we remind them that simulation is not about the simulator. As with simulations using SPs, manikin-based simulations require pre-work and investment of resources in the development of the simulation scenario itself. Pre-programmed scenarios will require time to download and perform testing before the scheduled simulation session. Simulator-based scenarios also require “suspension of disbelief” among learners and teachers alike.
With the right technology and environment, learners can work to develop and hone a particular skill until they’ve mastered it — without concern for real patient harm. If you feel your learners are ready to take part in full-fledged, high-fidelity simulation, your next steps may lead to a simulator.
While the learning curve will always exist in medicine, learners are afforded the opportunity to advance and gain competency through the use of simulation. Addressing topics like problem-solving, crisis-management, and hands-on procedures, each means of simulation provides deliberate practice of cognitive and psychomotor skills. Obstetrics and gynecology injuries are estimated to be involved in forty-three percent of malpractice claims exceeding five million dollars.18 With this in mind, it’s worth weighing the various ways to reduce the risk of patient harm and litigation.
In a randomized, controlled trial, the effectiveness of multi-professional training for eclampsia was measured in both local hospitals and a regional simulation center. At the hospitals, standardized patients were used in lower-fidelity simulation and, at the simulation center, a high-fidelity, full-body simulator was used. According to the British Journal of Midwifery, “there were equal improvements in both settings; it was the training itself, rather than the location or the simulation equipment used, that appeared to be the key to success”.19
Task trainers, standardized patients, hybrid simulation, and manikins have all proven to be enduring and invaluable training tools. When considering the best option for your needs, it comes down to identifying your desired educational outcome and understanding which model would best achieve your goal (knowledge acquisition, skills proficiency, decision-making, or simulation in teams). Regardless of the choice you make, you may improve your team’s skill levels so that they are better-prepared when real patient lives are at stake.
If you would like guidance on which level of fidelity will best meet your education and training needs, please contact us. We are here to help.