The following are both true stories that were circulated widely in the media. Both involved emergencies in the first moments of a child’s life…
In the first story, the attending staff had trained aggressively to identify and manage labor and delivery emergencies. Upon diagnosing the immediacy of the risk factors present, the staff carried out a well-planned and rehearsed effort that avoided harm to the child. To the joy of the family, the birth was a resounding success.
At a nearby facility a similar emergency occurred, but a different story was playing out. How the circumstances were diagnosed and addressed led to emergency interventions that proved fatal to the child and resulted in a $10.2 million award to the mother.
Worldwide each year, an estimated 814,000 neonatal deaths are related to intrapartum hypoxic events (i.e. “birth asphyxia”) in full-term infants.1 Of those that survive, many are left with neurological impairments.2
When a baby is born, he or she should begin breathing within the “Golden Minute,” their first 60 seconds outside of the womb. Most babies do begin breathing on their own. 10 million babies worldwide, however, will need assistance.3 Approximately 10% of newborns who do not breathe on their own will respond to drying, warming, clearing of the airways, and stimulation. And, 1% of non-breathing babies will need advanced methods of resuscitation, such as chest compressions and medication.4
To the family, 1% means everything. That 1% stands in the way of the child’s survival, and increases the chance of brain damage even if he or she does survive. The mother who trusts that she will receive the best possible care expects that her providers have been fully prepared for the 1% risk.
One Minute: Too Short to Do Anything?
The “Golden Minute” refers to the first 60 seconds of an infant’s life. Within these limited seconds, the infant should begin breathing on his or her own, or interventions must be started.
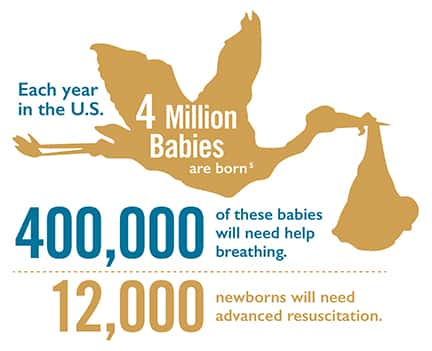
Approximately 4,000,000 babies are born each year in the United States.6 It is estimated that 400,000 of these babies will need help breathing and/or positive-pressure ventilations to successfully transition to extra-uterine life. And, as many as 12,000 infants will need advanced resuscitation with chest compressions and cardiac medications.7
In each case, steps taken to treat an infant must be precise and timely.