How Can Simulation Help Identify and Mitigate Latent Safety Threats?
An Interview with Jennifer McCarthy, MAS, NRP, CHSE-A
Director of Clinical Simulation at Seton Hall University and President/Founder of 579 Solutions



Jennifer: When we explore the uses of simulation for latent safety risk, it’s important to identify what we mean by that term. And we can pull information from Professor James Reason’s Swiss Cheese Model, where systems are aligned to allow errors to pass through and occur.
Currently, we spend a lot of time looking at processes after an error. … The use of simulation [allows us] to explore proactively where these latent risks are living so that we can eradicate them before near-sentinel or sentinel events.

Jennifer: I’ve observed firsthand how the simulations have shown data about where to store equipment so that we can change practice and have better outcomes. An example of that would be falls in the emergency department.
The other thing that I’ve observed firsthand is a change in practice, where we’re going to reduce the time from EMS acknowledgment in neurology cases to actual CAT scan diagnostic time. And practicing that before we go live so that the systems and safety measures are all in place, so that every clinician is safe – but mostly, our patients are safe.

Jennifer: There’s an important opportunity for us as a profession and working collaboratively with healthcare organization leadership to take the misnomer that we have bad people in healthcare delivery and that’s the cause of our patient safety issue.
We actually have excellent people who are caught in bad systems. This has been shown not only in the evidence for the last 25+years, but the 1999 report ‘To Err Is Human’ underscores this important point. And it’s important that we collectively embrace that for our clinicians and to achieve no harm.
It’s exciting right now in healthcare simulation to think about where we’ve been in the last 25 years and where we want to go, and then have the purposeful pursuit to make sure we travel where we want to be.
And one of the things that I’m curious about with latent risk assessment is, is there an opportunity to have bidirectional use – both from health systems to academic pre-licensure programs, where we’re working collaboratively to share information and address patient safety on a more collaborative level?

Jennifer: The adage that data drives the story and drives the outcomes can never be more true than when we’re looking at simulation and latent risk assessment. This data is not just qualitative with numbers and outcomes and reductions, but it is also the anecdotal storytelling of how these simulations were modifying the practices and raising the confidence of the clinicians to achieve better patient safety outcomes. And then of course, the storytelling from the perspective of the patient and what an amazing outcome they were able to achieve by the collective work that we’re all completing.
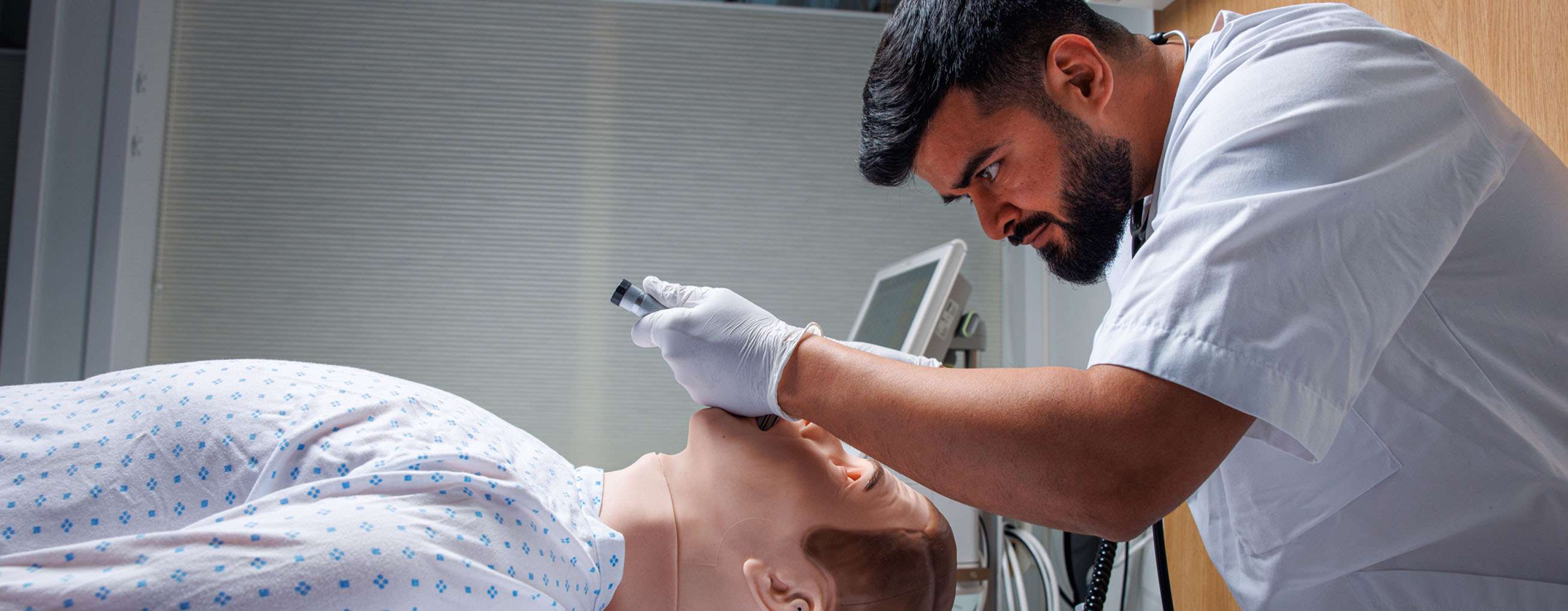
Jennifer: Simulation has been used for decades for intra-professional simulations, building practice within a profession.
It’s time now for us to think about examples where we can be collaborative with each other in an inter-professional model, which is how patients are holistically cared for.
And a couple of examples that I’ve had the gift of observing would be changing a rapid response team’s communication style by being side-by-side in simulation so that we’re using the correct acronyms and slowing down to actually honor everybody’s role in that rushed moment.
Jennifer McCarthy MAS, NRP, CHSE-A
Director of Clinical Simulation
Clinical Associate Professor
Seton Hall University
President and Founder, 579 Solutions
