Virtual SUN speakers(2)
Frontline leaders discuss the vital role of simulation in a COVID-19 response
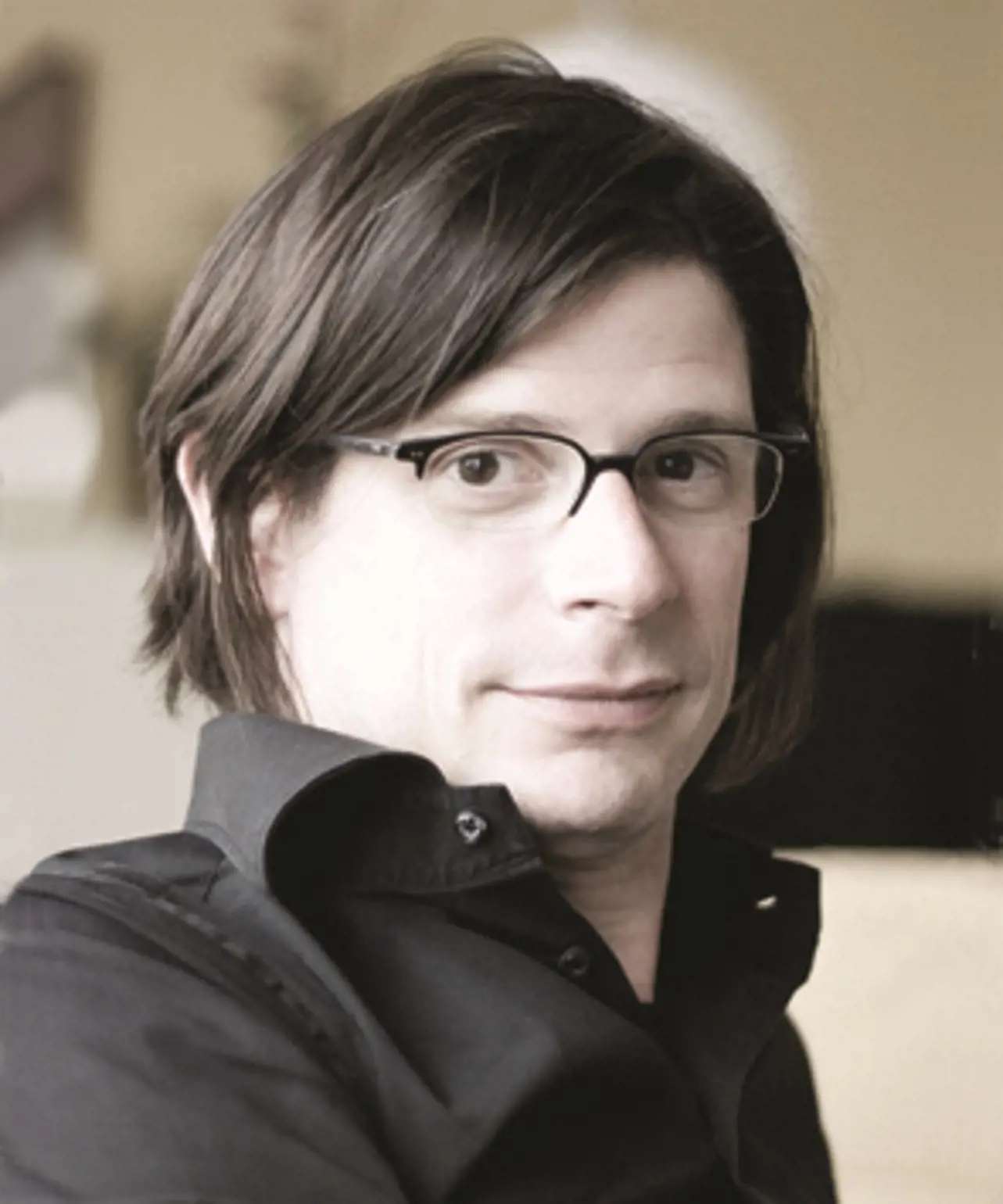 |
Dr. Peter DieckmannHead of Research, Copenhagen Academy for Medical Education and Simulation (CAMES), |
Dr Peter Dieckmann is a psychologist, who has worked with simulation since 1999, and focused on simulation in healthcare since 2001. He is currently Head of Research at the Copenhagen Academy for Medical Education and Simulation (CAMES). He received his PhD for his work on simulation in Anaesthesia in 2005.
Dr Dieckmann is driven to work with simulation, largely because it can lead to improved patient safety and quality of care. His areas of interest include research on simulation and research with simulation. His research on simulation contributes to a better understanding of how to use simulation for education, training and research (e.g. investigating debriefings as learning opportunities). His research with simulation uses simulation settings to explore performance-shaping factors, such as failures of prospective memory; how to use simulation to optimise health care failure modes and effects analyses; or how to use simulation to investigate the usability of medical products such as medication labels.
Conceptualising simulation as social practice, he is interested in simulation as both a tool for analysis and intervention. Dr Dieckmann is a Past President of the Society in Europe for Simulation Applied to Medicine (SESAM). He was Co-Chair of the International Meeting on Simulation in Health Care (IMSH) in 2011 in New Orleans, which attracted approximately 3,000 participants. Dr Dieckmann is also Associate Editor of the journal, Simulation in Healthcare.
 |
Sigrun Anna QvindeslandRegSim leader / Project lead Department of Research & Innovation |
Sigrun Qvindesland currently leads the preparations for establishing the Norwegian Simulation Network for Hospitals, the RegSim West regional simulation network.
She has worked in simulation since 2011 for the Stavanger University Hospital and SAFER center. Building on her clinical background as an emergency nurse practitioner, she worked as the hospital coordinator for simulation from 2011-2017. That position consisted of motivating, educating and supporting clinical simulation practitioners to run effective simulation-based educational initiatives both at the center, and in situ.
In situ team training, and working within organizations to ensure value-based simulation for all stakeholders are her key areas. This demands continually building and maintaining constructive working relationships and networks, across all levels and sectors of organizations.
 |
Kjetil TorgeirsenManager external training programs |
Kjetil Torgeirsen is Manager of external training programs and senior facilitator at SAFER simulation center in Stavanger, Norway.
He is an experienced simulation educator with international experience from faculty development programs in Russia and India. He is currently writing his master thesis in the pre-hospital critical care master’s program at the University in Stavanger and he also has an education in organizational leadership.
He has been working with medical simulation since 2006 and has been educating paramedics, nurses, physicians and medical teams for emergency medicine and patient safety.
 |
Dr. Nick MurchMB.BCh, PGCertMedEd, FHEA, MRCP |
Nick Murch is the Clinical Lead for Acute Medicine at the Royal Free Hospital, London where he also leads on team-based and part-task simulation as well as the in situ STEALTH team. He is an Honorary Clinical Associate Professor with UCL Medical School as well as the Acute Medicine Training Programme director for Acute Medicine in North Central and East London.
In his spare time, he is an author, coach and ultra-marathon swimmer who helps to train others for events such as swimming the English Channel. He is well known to be built for comfort and not for speed.
Nick was asked to join the Nightingale team for induction and education. His work encompassed clinical work as well as education and he became the in-situ simulation lead as well as working on the step-down area and discharge processes. He was a key member of the team who instigated the Day Zero simulation programme.
 |
Clinton JohnHead of Clinical Education Senior Operating Department Practitioner |
 |
Mark C. Henry, M.D.Professor and Chair |
Dr. Henry was one of the first residency-trained and Board Certified Emergency Medicine physicians to practice in New York City and New York State. As a member of the original Regional Emergency Medical Advisory Committee for New York City, he helped develop standards for EMS, 911- receiving hospitals, and specialty referral centers in an EMS system receiving over 1,000,000 calls annually.
Dr. Henry arrived at Stony Brook as Chairman of Emergency Medicine in 1990. He has led the department to national stature in the area of emergency medicine research. An avid EMS researcher, Dr. Henry has contributed to the scientific medical literature in the areas of public access defibrillation, pre-hospital response times, trauma triage, field trauma documentation, use of 12-lead ECG in the field, medical direction of EMS, airway management, IV catheter safety, and CPR/first aid training for the general public. He lectures nationally and internationally, including Israel, Korea, Portugal and Brazil, on emergency medicine and EMS related topics. Dr. Henry has authored many scientific publications, textbooks, chapters and curricula for emergency medicine and EMS. This includes a comprehensive textbook for Emergency Medical Technicians, "EMT Prehospital Care". Dr. Henry served as Chairman of the New York State Emergency Medical Advisory Committee and as Medical Director of the EMS Program for the New York State Department of Health for 17 years. During his tenure, research trials, clinical protocols, educational programs, legislative initiatives, and community based EMS programs such as defibrillators in public schools have significantly improved the effectiveness of the New York State EMS System.