How In Situ Simulation Can Reveal Latent Safety Threats in the ED


In healthcare the majority of quality issues stem not from individual errors but from systemic flaws that set the stage for failure. That may come as a surprise - and it requires a shift in how we think about quality. But as the late Dr. Lucian Leape, a pioneer in patient safety, famously stated:
In healthcare, a system is commonly defined as a coordinated network of people, processes, technologies, and settings that work together to deliver safe, effective, and patient-centered care. Systems issues often manifest themselves as latent safety threats: hidden problems in equipment, environment, processes, or communication that lie dormant until they contribute to harm.
In situ simulation, or simulation conducted in an actual care environment, has emerged as a powerful tool not only for training but also for uncovering these threats before they reach the patient. By recreating real-world clinical scenarios, in situ simulation allows teams to surface vulnerabilities that would otherwise go unnoticed. This provides a unique lens into the quality and reliability of healthcare delivery systems.
The complex, high-pressure environment of the Emergency Department (ED) makes it especially vulnerable to latent safety threats (LSTs).3 Often referred to as “accidents waiting to happen,” LSTs are system issues that aren’t immediately apparent and can make it easier for healthcare providers to make errors.
In this article, we explore how you can use in situ simulation to help uncover LSTs and drive quality improvement in your ED.

In situ simulation gives you a unique opportunity to stress-test your system, because it takes place in the actual clinical setting.
Dr. Andrew Petrosoniak, MD, MSc (Med Ed), FRCPC, Emergency Physician and Trauma Team Leader at St. Michael’s Hospital in Toronto, Canada, compares in situ simulation to crash testing a car.5
“You can imagine that no car company is ever going [to] roll out a car that hasn’t been crash tested,” he points out. “It's not sufficient to just drive it around the neighborhood and say that it’s safe. It needs to be put through a collision. In simulation, it’s the exact same process. We can replicate systems, processes, [and] we can study physical spaces much better using simulation and understand exactly how things will work before a patient ever arrives.”
Read on to explore 4 common LSTs that EDs have uncovered and resolved using in situ simulation.

In situ simulation scenarios allow providers to practice the entire process of medication administration, from prescription to dispensing to administration to the patient.
Common medication LSTs that simulation has identified include:
The Pediatric ED at the Cincinnati Children’s Hospital Medical Center conducted 90 in situ simulations.7 They discovered 73 LSTs – and 30% of them were related to medication safety, including:
Another ED in Canada initiated an in situ simulation program to identify LSTs as part of a quality improvement project.8 Through the simulations, they found 158 LSTs – with medication issues accounting for 1 in 5 of them. LSTs included:
If medication errors are your concern, you may wish to consider our SimMan® 3G PLUS, SimMan Critical Care, SimMan Trauma, or any of our other high fidelity simulators that have RFID radio frequency identification.

Equipment is often a proximate cause. A 2024 literature review on in situ simulation in emergency medicine found that 83% of the LSTs identified were related to equipment issues.9
We already mentioned critical medications missing from Pyxis machines. Add to that potential unfamiliarity with electrocardiogram (ECG) machines, multiparameter monitors, pulse oximeters, blood pressure monitors, portable X-ray machines, ultrasound, defibrillators and more. There is a lot for ED personnel to manage.
One of the greatest benefits of in situ simulation is that it allows you to use your own equipment. In doing this, many hospitals have found issues with:
![]()
Not knowing the location of equipment, resulting in delays to care
![]()
Not having equipment organized in a specific area
![]()
Equipment not working
![]()
Equipment missing
In one study consisting of 18 in situ simulations performed across 11 EDs, participants uncovered a total of 158 LSTs - 25% of which were related to equipment,10 including:
![]()
Equipment not easily accessible, including central line and chest tube
![]()
Equipment failure, including a failing laryngoscopy light and transvenous pacer balloon
![]()
Non-appropriate equipment identified, including equipment that was out-of-date
Simulations can also be tailored to specifically include medical equipment malfunctions. This allows providers to practice their response to such situations, identifying LSTs related to equipment reliability, maintenance issues, and potential consequences for patient care.
Struggling to envision how to document and track equipment issues? Try using our SimCapture platform- it allows you to record video, collect data, and evaluate real-time performance with ease.

Dr. Andrew Petrosoniak shared how his hospital used simulation to drastically improve their massive transfusion protocol in the ED.11 By simulating the protocol in the actual environment of the ED, he and his staff uncovered issues including:
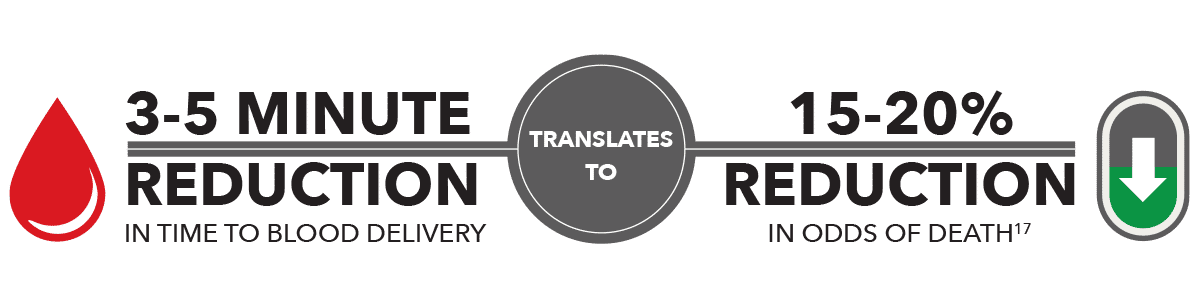
To mitigate the issues found, they streamlined their process to order blood and educated the porters on the crucial nature of receiving blood rapidly for a trauma patient. When they later measured how their protocol adjustments were translating to actual patient care, they found some amazing results:
This example illustrates that utilizing simulation to expose and improve systems issues like inadequate protocols can make a substantial impact on patient care.
In this arena, it is especially helpful to use a system like SimCapture coupled with SimMan 3G PLUS, SimMan Critical Care, or any other of our high-fidelity simulators that can give you detailed feedback on how a change in protocol can impact a patient’s condition.

In a complex and high-stress environment like the ED, strong teamwork, especially interprofessional teamwork, is critical.13 In situ simulation provides a risk-free environment to bring everyone together to practice as a practice as a team in the same space they work in daily. A well-designed simulation scenario followed by a thorough debriefing can identify LSTs related to miscommunication, misunderstandings, or breakdowns in communication among different members of the healthcare team.
When you think about the types of scenarios in which solid teamwork is of the utmost importance, codes may come to mind. One study used in situ simulation to study resuscitations in the trauma bay of the ED.15 They used a SimMan 3G simulator and recorded all the scenarios to facilitate careful debriefing and review.
They uncovered 843 LSTs during 12 simulations.16 Fifty percent of them involved teamwork and communication, and many of the LSTs were categorized as critical threats.
LSTs included:

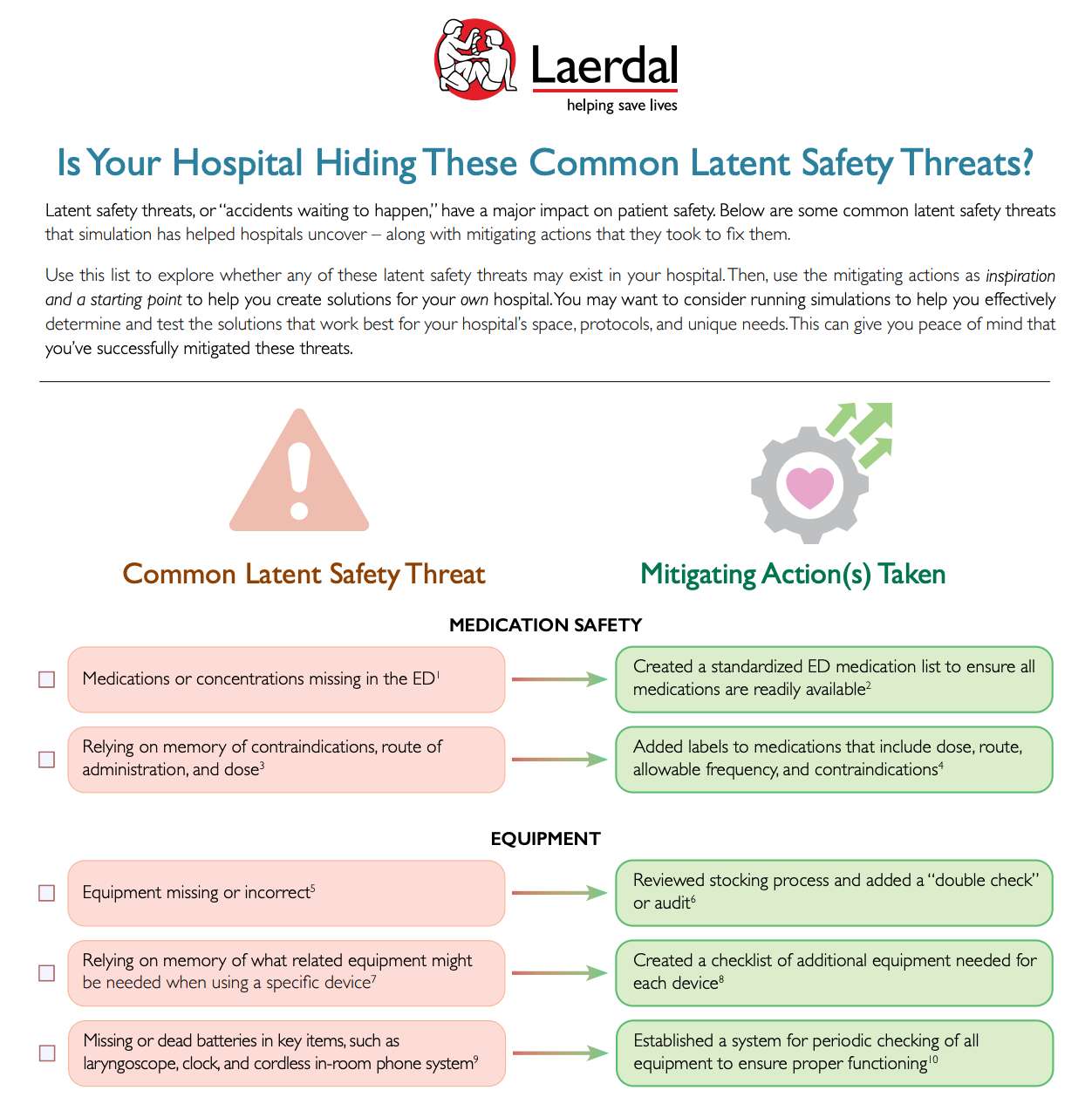
Download this checklist of common LSTs and how organizations have solved them, so that you can explore these areas in your own organization.
References
1. Harvey, H. B., & Sotardi, S. T. (2017). The Just Culture Framework. Journal of the American College of Radiology, 14(9), 1239–1241. https://doi.org/10.1016/j.jacr.2017.04.030
2. Leape, L. L. (2009). Errors in medicine. Clinica Chimica Acta, 404(1), 2–5. https://doi.org/10.1016/j.cca.2009.03.020
3. O’Dochartaigh, D., Ying, L., Simard, K., Eichorst, C., Kaba, A., Mews, L., Chan, M., Brown, T., Kirkham, A., & Ma, W. (2022). Identifying and managing latent safety threats though a zone-wide emergency department in-situ multidiscipline simulation program: A quality improvement project. Canadian Journal of Emergency Nursing, 45(2), 37–46. https://doi.org/10.29173/cjen157
4. Long, J. A., Webster, C., Holliday, T., Torrie, J., & Weller, J. (2022). Latent safety threats and countermeasures in the operating theater. Simulation in Healthcare : Journal of the Society for Simulation in Healthcare, 17(1), e38–e44. https://doi.org/10.1097/sih.0000000000000547
5. Gardner, E. & De Souza, P. (Hosts) (n.d.). In Conversation with Dr. Andrew Petrosoniak. (No. 5) [Audio podcast episode]. In Healthcare Change Makers Podcast. HIROC.
6. Nguyen, P. T. L., Phan, T. A. T., Vo, V. B. N., Ngo, N. T. N., Nguyen, H. T., Phung, T. L., Kieu, M. T. T., Nguyen, T. H., & Duong, K. N. C. (2024). Medication errors in emergency departments: a systematic review and meta-analysis of prevalence and severity. International Journal of Clinical Pharmacy, 46. https://doi.org/10.1007/s11096-024-01742-w
7. Patterson, M., Geis, G. L., Falcone, R. A., LeMaster, T., & Wears, R. L. (2012). In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Quality & Safety, 22(6), 468–477. https://doi.org/10.1136/bmjqs-2012-000942
8. O’Dochartaigh, D., Ying, L., Simard, K., Eichorst, C., Kaba, A., Mews, L., Chan, M., Brown, T., Kirkham, A., & Ma, W. (2022). See reference #3.
9. Grace, M., & Róisín O’Malley. (2023). Using In Situ Simulation to Identify Latent Safety Threats in Emergency Medicine. Simulation in Healthcare : Journal of the Society for Simulation in Healthcare. https://doi.org/10.1097/sih.0000000000000748
10. O’Dochartaigh, D., Ying, L., Simard, K., Eichorst, C., Kaba, A., Mews, L., Chan, M., Brown, T., Kirkham, A., & Ma, W. (2022). See reference #3.
11. Gardner, E. & De Souza, P. (Hosts) (n.d.). See reference #5.
12. Ibid.
13. Milton, J., M. Gillespie, B., Åberg, D., Erichsen Andersson, A., & Oxelmark, L. (2022). Interprofessional teamwork before and after organizational change in a tertiary emergency department: An observational study. Journal of Interprofessional Care, 37(2), 1–12. https://doi.org/10.1080/13561820.2022.2065250
14. Petrosoniak, A., Auerbach, M., Wong, A. H., & Hicks, C. M. (2016). In situ simulation in emergency medicine: Moving beyond the simulation lab. Emergency Medicine Australasia, 29(1), 83–88. https://doi.org/10.1111/1742-6723.12705
15. Petrosoniak, A., Fan, M., Hicks, C. M., White, K., McGowan, M., Campbell, D., & Trbovich, P. (2020). Trauma Resuscitation Using in situ Simulation Team Training (TRUST) study: latent safety threat evaluation using framework analysis and video review. BMJ Quality & Safety, bmjqs-2020-011363. https://doi.org/10.1136/bmjqs-2020-011363
16. Ibid.