Can Simulation-Based Team Training Reduce Sick Leave Rates?
A recent study uncovered a strong connection between simulation team training and sick leave.

A recent study uncovered a strong connection between simulation team training and sick leave.

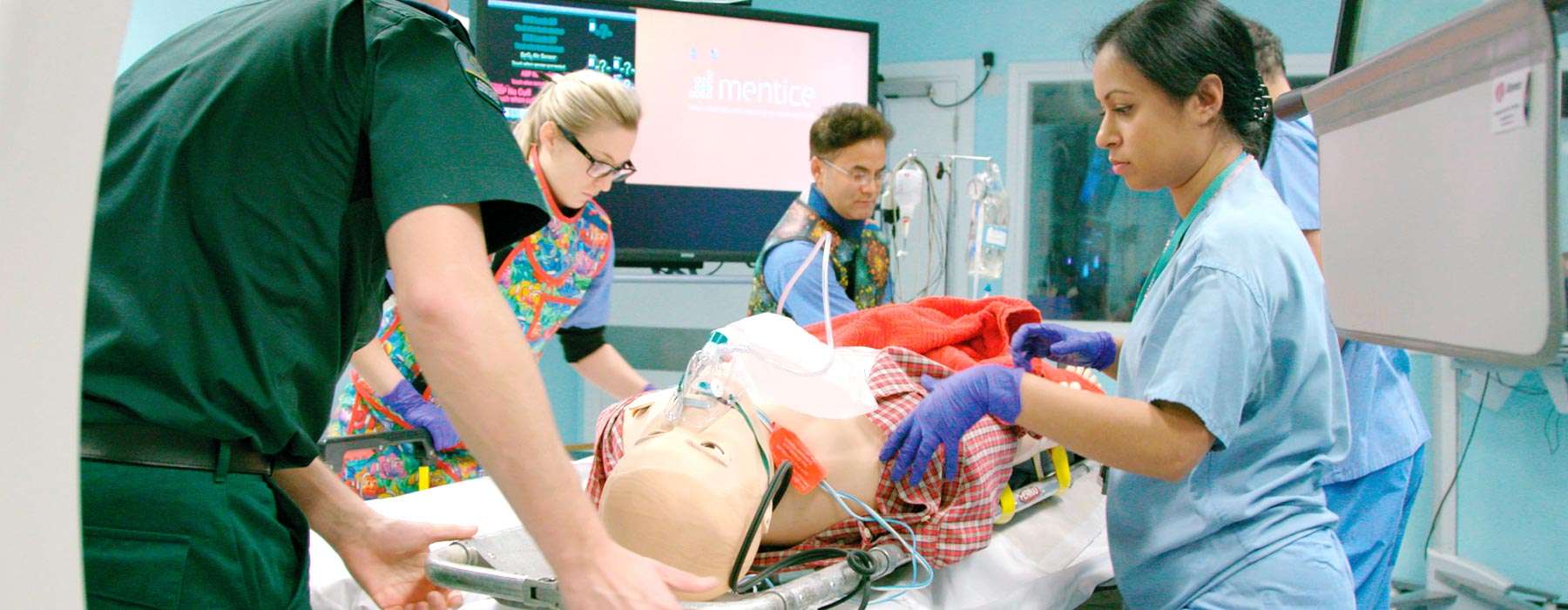
Simulation-based team training is well-known to improve team dynamics in healthcare.1 These hands-on, realistic training experiences foster the collaboration, coordination, and effective communication that are critical to establishing high-performance teams.2
A recent research study is shining light on another possible benefit of simulation-based team training: it may have a protective effect on employee wellbeing.3
In this article, we provide you with highlights from the study, as well as some additional research related to the findings.

The 2023 study looked at the relationship between simulation-based team training and sick leave rates across 5 hospitals in Denmark over a 5-year period (2015-2020).
The intervention group consisted of 14,872 clinicians from 2 hospitals. The clinicians participated in 210 simulation-based training sessions between 2017-2019.
The simulation scenarios included both technical and nontechnical learning objectives.
involved managing high-acuity situations including:
Cardiac arrest
Anaphylaxis
Managing the difficult airway
Transportation
involved key elements of effective team dynamics, including:
Closed-loop communication
Leadership
Resource Management
The study also included a control group, which is rare among studies that investigate the benefits of simulation-based team training.4 The control group consisted of 3 hospitals that performed minimal simulation training activities during the study period.
The researchers compared the intervention group’s sick leave rates before vs. after the simulations. They also looked at sick leave rates in the control group over the same period.
The results
The results of the study found that both the control group and the intervention group had increases in sick leave over the study period. However, the increase in sick leave rate was statistically significantly lower in the intervention group.
Measuring the effectiveness of a simulation program can be challenging. In many studies, Likert scales are used to measure whether the participant felt that the training was valuable or believes that their skills have improved, vs. looking at the effect on clinical outcomes or other objective factors.5 Likert scales present participants with a statement and asks them to rate the extent to which they agree with it, using values ranging from “strongly agree” to “neutral” to “strongly disagree.”6
In this study, sick leave rates substantively take the place of a Likert scale or other measures. The reduction in sick leave is an objective, tangible indicator of the impact that simulation likely had on the employees.

How exactly might simulation-based team training have made an impact on the clinicians’ sick leave rates? One likely explanation involves stress – and how it’s connected to team relationships.
The study points out that simulation-based team training fosters strong professional connections and a supportive work environment. These benefits, the study explains, may act as "vital buffers" against chronic stress.
While definitions of stress vary across the literature, stress can generally be described as “what arises when something you care about is at stake."7 Stress has been found to be a key factor associated with sick leave in healthcare.8 And, prolonged periods of high stress often lead to burnout.9
Clinicians' feelings about the quality of their team interactions play a considerable role in their stress levels.10
And, research from 2021 found that healthcare professionals who felt like they were part of a team had significantly less work stress and burnout.12
These factors help explain how simulation-based team training can make an impact on sick leave rates. The increased communication, collaboration, and other teamwork elements that clinicians gain through simulation can help protect them from some of the stress that contributes to sick leave rates.
The bottom line
If your healthcare organization is like many others, your clinicians are likely dealing with high levels of stress and burnout in this increasingly complex healthcare environment.
Simulation-based training may not be the first thing that comes to mind when it comes to thinking about ways to reduce stress and burnout in the workplace. But the evidence is clear: teamwork quality is an important factor in clinicians’ wellbeing. Simulation-based team training can help them foster the skills, confidence, and strong relationships they’re looking for.
Simulation will not only help your clinicians make a positive impact on patient outcomes through enhanced teamwork – but it may likely protect their wellbeing, too.
If you’re interested in using simulation-based training to strengthen team performance – and potentially your teams’ wellbeing – Laerdal can help.
Our mission at Laerdal is Helping Save Lives. One of the ways we pursue that mission is to ensure that clients can use simulation-based training and education to prepare their staff to deliver the best possible patient outcomes regardless of the acuity of the case. Our goal is to help save an additional 1 million lives annually by the year 2030.
Contact your Laerdal representative today so we can begin a discussion on how we can best support you.