
Using Simulation to Build High Performance Teams
Many organizations have begun implementing initiatives to support better patient safety. Training multidisciplinary teams through the use of simulation is proven to reduce patient risk.
As July approaches, medical students brace themselves to begin their intern residency programs. In 2022, the National Resident Matching Program's Main Residency Match included 39,205 total positions - the largest number in history.1 This marks a continued annual growth in new resident positions in America.
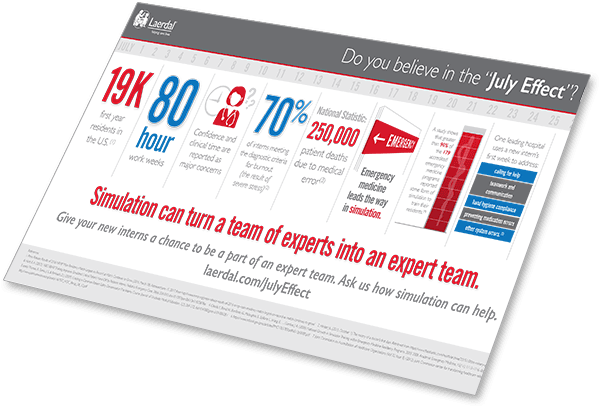
For some patient safety advocates, this raises a repeated concern about the so called "July Effect", a potential increase in medical error during July as new interns assume their new roles as practitioners and as leaders.
Medical errors can be defined as:2
While some studies argue that the "July Effect" marks an increased risk to the care of patients, others indicate no effect at all. Conflicting data aside, introducing new team members to an established hospital workforce at any time has the potential to affect daily operations, morale, and even patient outcomes.
With the change of guard [each July] come new questions, new relationships, and a generation of our country’s brightest minds quickly understanding that they are real doctors.
For interns, this transition means making a leap from the breadth of information needed to graduate from medical school to practicing a narrow set of skills just to perform daily tasks. Dr. Matt McCarthy, author of The Real Doctor Will See You Shortly: A Physician's First Year, reflects that if he had been asked to "recite pages from a journal article on kidney chemistry or coagulation cascades, I could've put on quite a show...But I hadn't learned much of the practical business of keeping people alive – skills like drawing blood or putting in a urinary catheter".4 One solution to avoid the "July Effect" is to use simulation to minimize the learning curve for greater control and efficiency.
Drawing on the experience of experts, in this article we share five insights about where and how you can use simulation to support your new resident interns as they transition to practice. We discuss:
Using simulation in residency programs is not a new concept. As early as 2008, greater than 90% of the then 179 accredited emergency medicine programs in the U.S. reported the use of some form of simulation to train their residents, with 85% specifically using manikin-simulators.5
Practicing safe medicine continues to depend on the acquisition of medical knowledge, proper judgment, and practical skill. And, with stricter clinical governance and a greater focus on patient safety, acquiring these skills before independent practice is challenging for residents.6
A study conducted by Magee-Women’s Hospital of University of Pittsburgh Medical Center concluded that simulated patient exercises can be utilized in multiple arenas to teach OB/GYN residents communication skills, while simultaneously addressing their clinical knowledge deficits.7 In another study conducted by Johns Hopkins University, simulation training was used to improve critical patient hand-offs by pediatric interns.8
New interns often find themselves in situations where their role can be crucial to avoiding preventable harm. To address this, many facilities, including Massachusetts General Hospital and Yale-New Haven Hospital, have implemented longer and more robust training for interns. Despite questioning the legitimacy of a “July Effect”, doctors and administrators working in these hospitals support sensible precautions which include interns completing simulations, task training, and online learning.11
Similarly, the University of Miami-Jackson Memorial Hospital Center for Patient Safety now uses a blended learning approach that involves lecture, web-based learning, and small group simulation.
If these or any other patient safety issues are your concern, even basic simulations can address them and turn practice into permanence.
At this point you might be asking:
If these are your concerns, perhaps you may wish to consider using in situ (i.e. on site) simulation in the very environment in which your new interns will practice.
Residents typically have no prior experience, yet are expected to diagnose and treat patients in these unfamiliar settings.13 And, "[they] are unfamiliar with their new working environment, equipment, hospital layout, and culture, which can cause anxiety," according to Dr. Chopra and Dr. Kondapalli of Iowa State University. A cardiac arrest, for example, is no time to be discovering functionality of your defibrillators, layout of your crash carts, or how to activate a code. It's equally no time to be discovering your protocol, processes, and procedures.
As a solution, in situ simulation can effectively introduce interns to their new work environments. And, since new interns will be dependent on working with teams, in situ simulation allows everyone to review and reinforce their skills, all the while identifying hazards and deficiencies in their systems and environment.14
Interns will work with a mix of individuals including nurses, senior residents, physicians, paramedics, and personnel who they may not get the chance to know on a personal level. Understanding how to manage team dynamics despite who is on the team becomes an important asset. Great teams know this and that's where they focus – not just on refining individual skills but on instilling the skills necessary to excel within teams.15
In particular, simulation offers benefits that outpace didactic learning, such as:
In their paper, "Emergency Medicine Simulation: A Resident's Perspective", Drs. Meguerdichian, Heiner, and Younggren describe a new resident stepping into an emergency department (ED), immediately confronted by the commotion of a team trying to save a patient who has begun to code. The new resident quickly determines that the patient needs to be intubated. The airway proves to be difficult, and with every step the new intern takes, first using a Macintosh blade, then a video laryngoscope, the patient deteriorates one step ahead. Alarms blaring, and sweat building up on his brow, the new intern prepares to perform a cricothyroidotomy. With that decision, the alarms halt, and the new intern is commended for his efforts. The case was a simulation, part of what all three doctors encourage as part of an onboarding process for new residents.16
This type of situation, a low frequency, high acuity event, can be especially problematic for a new intern given the infrequency of true hands-on practice.17 Simulation provides the necessary experience - without putting a patient at risk.
Three leading indicators of good patient-centered performance are staff confidence, competence, and compliance. Yet, interns can reportedly feel paralyzed in the first year of their residency program as they adjust to the change in their environment and an awareness of how much there is to learn. "I spent much of [my first year] in a state of crisis and doubt," says Dr. Sandeep Jahuar, author of the memoir Intern.20
Incorporating simulation in your program will not only benefit the new interns but will give attending physicians a chance to gauge resident confidence, competency and compliance with hospital regulations, their new environment, and their new teams – all while protecting the patient.