2022 Looking Forward: What to Expect in Nursing Education
A summary of what we're seeing - plus some guidance to help

A summary of what we're seeing - plus some guidance to help

The U.S. Bureau of Labor Statistics projects the need for 1.1 million new RNs in 2022.1 Contributing factors include increased demand for care during the pandemic, nurse burnout, an aging population with complex medical needs, and retiring nurses and faculty.2 In September 2021, the American Nurses Association urged the U.S. Department of Health and Human Services to declare the current situation a national crisis.3
This shortfall isn’t for lack of interest in entering the nursing profession. 80,521 applicants were turned away by nursing schools in 2020 due to insufficient numbers of faculty, clinical sites, classroom space, clinical preceptors, and budget constraints.
Looking ahead, more nursing programs are turning to simulation to help them do more with less so they can continue to meet an urgent need. Below, we share how simulation in nursing education is playing a role in helping schools produce practice-ready nurses in 2022.
With the pandemic still ongoing, clinical experiences may continue to be limited due to COVID-19 patients, overwhelmed nurses, and other issues.5
With all the uncertainties surrounding the future of the pandemic, many nursing programs are growing their simulation programs to provide a safety net from the scarcity of clinical site opportunities. And, educators are increasingly realizing the value of the nursing simulation lab in creating a risk-free hands-on learning environment.

Dr. Desiree Hensel, Dean of Curry College School of Nursing6
If one of your many worries is having enough clinical time for your students, you may want to consider growing your simulation program to provide assurance that hands-on opportunities are consistently available.
First and foremost, find out your Nursing Regulatory Body (NRB)’s education requirements for use of simulation in your state. Begin by referencing the NCSBN’s state-by-state education requirements document – but always be sure to check with your state for any updates. Then, consider investing in a simulator that is often used for replacing clinical time in nursing programs.
Nursing Anne Simulator is a common choice for covering core nursing skills, and its modularity allows it to simulate a variety of patients.
New data suggests that rates of preparedness in new nurse graduates are declining.
At the same time, schools are still battling faculty shortages. In a 2019 survey from the American Association of Critical-Care Nurses, nursing schools reported that faculty shortages were the top reason for not accepting more applicants into their programs.8 And, one third of nurse faculty in baccalaureate and graduate programs are expected to retire by 2025.9
These factors point to the need for efficient processes that ensure consistent, quality learning experiences, while identifying and addressing learning improvement needs early.
When considering the difference that an efficient process can make, think about a totally different industry, manufacturing. Manufacturers must ensure that every unit they produce is of consistent quality, with minimal wasted time or effort in the process. To accomplish this, many of these companies use data-driven process improvement and quality control approaches. These approaches involve measuring and analyzing data to uncover causes of variation and poor performance so that they can be improved. The healthcare field sometimes uses similar processes to identify and eliminate the causes of medical errors and to mitigate variability in care.10
When paired with careful measurement and assessment of performance data, simulation can help create a similar level of efficiency. Simulations ensure that each student gets the same quality consistent experience. Performance data insights can help uncover individual or cohort-level issues early so they can be ironed out immediately. The result? An efficient “manufacturing” process that churns out confident, prepared future nurses.
If you're interested in increasing efficiency in your simulation program, the SimCapture simulation learning management system can help make it possible by facilitating the management, recording, and assessment of your simulation training. Easy-to-use reports and statistics on performance can help track usage, KPIs, and learning outcomes. This will make it easier for you to make informed decisions and increase you organization's simulation return on investment.
The ongoing adoption of technology in nursing education was accelerated by the pandemic as programs shifted rapidly to new and innovative ways of teaching. This situation illustrated the power of using simulation in various forms to strengthen clinical skills.
Looking ahead, many programs plan to continue embracing simulation and other technologies to facilitate both in-person and online learning. In a 2020 survey on future technology trends in nursing education, responses from 450 nursing administrators, faculty, and deans found that 39% plan to offer more online courses post-pandemic.11 48% of respondents intend to invest more in virtual simulation in the next 2 years, while 34% plan to invest more in high-fidelity manikins.12
With more programs increasingly using multiple forms of simulation, some simulation centers are implementing approaches to help organize and align their simulation activities with learning pathways. The SimZones framework is one such approach. Originally developed for the Boston Children’s Hospital Simulation Program, SimZones is a system for matching simulation delivery methods to specific learning needs.13 It separates simulation activities into four zones, with the learning goals increasing in complexity as students progress through each zone.
The first zone involves independent auto-feedback exercises, often using virtual simulation, while the next zone covers hands-on foundational clinical skills. Students then move on to acute situational simulations, followed by team and system development simulations. In the final zone, students practice in real patient care settings. This phased simulation learning journey allows students to “walk before they run” and build upon what they’ve learned before reaching a real patient.
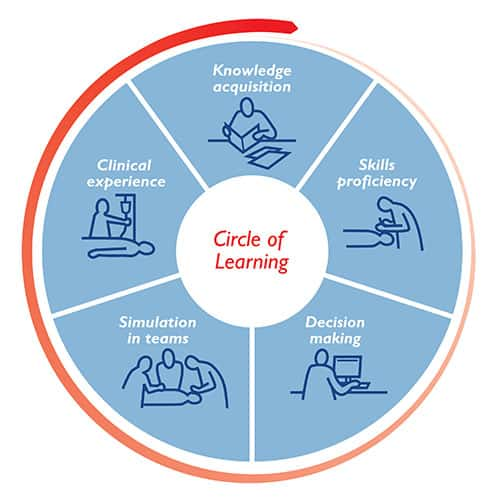
Laerdal has created its own modified framework for organizing the learning progression with our Circle of Learning. This systematic approach to healthcare training shows the phases of learning required to develop confidence and competence to effectively treat patients.
Efficiency will be key to building for better outcomes in 2022. Consider using the Circle of Learning to help you identify and address any missing pieces that might exist in your program. You may want to look for options that can also help you deal with other issues like shortages in space, faculty, or clinical time. Here are a few of our predictions for how our clients will be using simulation to address some of the segments within the Circle of Learning in 2022:
Laerdal Scenario Cloud
Find hundreds of high-quality, expert-validated scenarios made ready for you.
SimCapture
SimCapture allows you to effectively manage, record, and assess simulation training, both on-site and in-situ.
vSim® for Nursing
Develop clinical reasoning skills, competence, and confidence in nursing students with vSim for Nursing.
SimMan® 3G PLUS
Built on decades of expertise, SimMan 3G PLUS offers a fully immersive simulation experience with heightened realism.
Nursing Anne Simulator
Nursing Anne Simulator is a modular platform consisting of a variety of accessories and interchangeable parts that facilitate a variety of simulated patients and provide unique training opportunities.
Premature Anne
Developed in collaboration with the AAP, Premature Anne is designed to facilitate training of healthcare professionals in proper care and resuscitation techniques for preterm infants.
Educational Services
Our educational portfolio will help you to implement best practices in your simulation training to optimize learning potential in your students.
Technical Services
Prolong the life-span of your simulation equipment with follow-up services from Laerdal Technical Services.
Managed Services Program
With our Managed Services Program, we provide you with a flexible and sustainable solution designed to meet your organization's unique needs and ensure success.